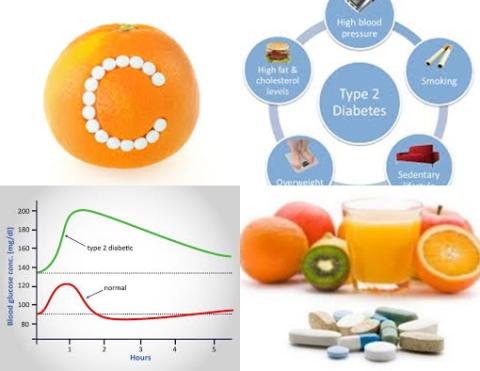
Higher concentrations of carotenoids reduce type 2 diabetes

Objectives:
Previous meta-analysis studies have indicated inverse associations between some carotenoids and risks of metabolic syndrome, cardiovascular disease, cancer and all-cause mortality. However, the results for associations between carotenoids and type 2 diabetes (T2D) remain inconsistent and no systematic assessment has been done on this topic. Therefore, this review article (meta-analysis) has been conducted.
Do higher dietary intakes and circulating concentrations of carotenoids reduce risk of type 2 diabetes?
Study design:
This review article included 13 studies.
Results and conclusions:
The investigators found for the the highest versus the lowest categories of dietary intake of β-carotene a significantly reduced risk of 22% for type 2 diabetes [pooled RR = 0.78, 95% CI = 0.70 to 0.87, I2 = 13.7%, n = 6].
This significantly reduced risk was also found for total carotenoids (n = 2), α-carotene (n = 4), and lutein/zeaxanthin (n = 4), with pooled RRs ranging from 0.80 to 0.91, whereas no significant associations were observed for β-cryptoxanthin and lycopene.
The investigators found for the the highest versus the lowest categories of circulating concentration of β-carotene a significantly reduced risk of 40% for type 2 diabetes [pooled RR = 0.60, 95% CI = 0.46 to 0.78, I2 = 56.2%, n = 7].
This significantly reduced risk was also found for total carotenoids (n = 3), lycopene (n = 4), and lutein (n = 2), with pooled RRs ranging from 0.63 to 0.85, whereas no significant association was found for circulating concentrations of α-carotene and zeaxanthin when comparing extreme categories.
The investigators found dose-response analysis indicated that nonlinear relations were observed for circulating concentrations of α-carotene, β-carotene, lutein and total carotenoids [all p-nonlinearity 0.05], but not for other carotenoids or dietary exposures.
The investigators concluded that higher dietary intakes and circulating concentrations of total carotenoids, especially β-carotene, are associated with a lower risk of type 2 diabetes. More studies are needed to confirm the causality and explore the role of foods rich in carotenoids in prevention of type 2 diabetes.
Original title:
Dietary Intake and Circulating Concentrations of Carotenoids and Risk of Type 2 Diabetes: A Dose-Response Meta-Analysis of Prospective Observational Studies by Jiang YW, Sun ZH, [...], Pan A.
Link:
https://pubmed.ncbi.nlm.nih.gov/33979433/
Additional information of El Mondo:
Find more information/studies on carotenoids and diabetes right here.