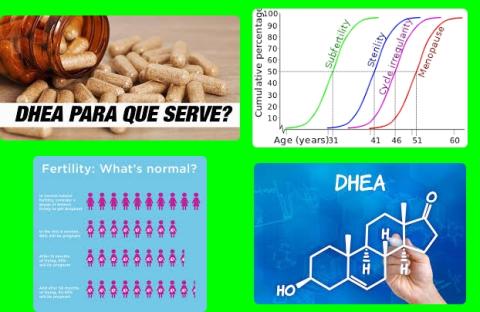
75 mg daily DHEA supplements increase fertility in women
Objectives:
Does dehydroepiandrosterone (DHEA) supplementation improve the outcomes of in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI) in women with diminished ovarian reserve (DOR) and/or poor ovarian response (POR)?
Study design:
This review article included 9 RCTs, published between 2010 and 2017.
The sample sizes ranged from 24 to 208, with a total of 862 patients.
All of included patients had been diagnosed with diminished ovarian reserve (DOR) and/or poor ovarian response (POR).
The treatment intervention was 75 mg daily DHEA versus placebo.
The lack of significant asymmetry of funnel plot indicated the lack of potential publication bias in the included studies.
Results and conclusions:
The investigators found in a pooled analysis using the random effects model revealed a statistically significant increase in retrieved oocytes in the DHEA group, compared to the control group [MD = 0.91, 95% CI = 0.23 -1.59, p = 0.009, I2 = 53%, p = 0.06].
The investigators found in 8 studies (405 in the DHEA group and 415 in the control group) a statistically significant increase in the clinical pregnancy rate in the DHEA group compared to the control group [RR = 1.27, 95% CI = 1.01 -1.61, p = 0.04, I2 = 0%, p = 0.57].
The investigators found in 5 studies (189 in the DHEA group and 190 in the control group) a statistically significant increase in the live birth rate in the DHEA group, compared to the control group [RR = 1.76, 95% CI = 1.17 -2.63, p = 0.006, I2 = 0%, p = 0.43].
The investigators found in 3 studies (96 in the DHEA group and 99 in the control group) no significant difference in the miscarriage rates between the DHEA and control groups [RR = 0.37, 95% CI = 0.12-1.13, p = 0.08, I2 = 25%, p = 0.26].
The investigators concluded 75 mg daily DHEA supplementation increases the retrieved oocytes, clinical pregnancy rate and live birth rate in women with diminished ovarian reserve and/or poor ovarian response, who are undergoing in vitro fertilization or intracytoplasmic sperm injection.
Original title:
The Effect of Dehydroepiandrosterone (DHEA) Supplementation on IVF or ICSI: A Meta-Analysis of Randomized Controlled Trials by Xu L, Hu C, […], Li Y.
Link:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6620181/
Additional information of El Mondo:
Find more information/studies on pregnancy right here.
Your body naturally produces the hormone dehydroepiandrosterone (DHEA) in the adrenal gland. In turn, DHEA helps produce other hormones, like testosterone and estrogen. Natural dehydroepiandrosterone levels peak in early adulthood and then slowly fall as you age.