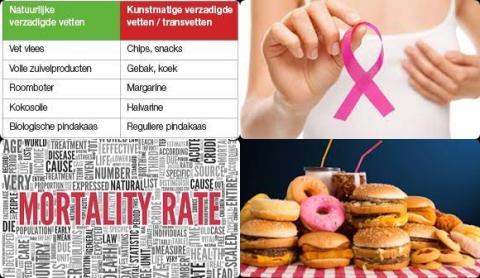
High consumption of dietary trans fat increases prostate cancer and colorectal cancer
Objectives:
Apart from ruminant fat, trans fatty acids are produced during the partial hydrogenation of vegetable oils, (eg, in the production of ultraprocessed foods). Harmful cardiovascular effects of trans fatty acids are already proven, but the link with cancer risk has not yet been summarized. Therefore, this review article has been conducted.
Does high consumption of dietary trans fat increase risk of cancer?
Study design:
This review article included 17 cohort and case-control studies on breast cancer, 11 cohort and case-control studies on prostate cancer and 9 cohort and case-control studies on colorectal cancer.
Results and conclusions:
The investigators found that high consumption of dietary total trans fat significantly increased prostate cancer with 49% [OR = 1.49, 95% CI = 1.13 to 1.95].
Significantly means that there is an association with a 95% confidence.
The investigators found that high consumption of dietary total trans fat significantly increased colorectal cancer with 26% [OR = 1.26, 95% CI = 1.08 to 1.46].
Significant because OR of 1 was not found in the 95% CI of 1.08 to 1.46. OR of 1 means no risk/association.
The investigators found no association between high consumption of dietary total trans fat and the risk of breast cancer [OR = 1.12, 95% CI = 0.99 to 1.26].
No association ant because OR of 1 was found in the 95% CI of 0.99 to 1.26. OR of 1 means no risk/association.
The investigators found results were dependent on the fatty acid subtype, with even cancer-protective associations for some partially hydrogenated vegetable oils.
The investigators found enhancing moderators in the positive transfat-cancer relation were gender (direction was cancer-site specific), European ancestry, menopause, older age and overweight.
The investigators concluded that high consumption of dietary total trans fat increases prostate cancer and colorectal cancer. Future studies need methodological improvements (eg, using long-term follow-up cancer data and intake biomarkers). Owing to the lack of studies testing trans-fatty acid subtypes in standardized ways, it is not clear which subtypes (eg, ruminant sources) are more carcinogenic.
Original title:
Dietary trans-fatty acid intake in relation to cancer risk: a systematic review and meta-analysis by Michels N, Specht IO and Huybrechts I.
Link:
https://pubmed.ncbi.nlm.nih.gov/34104953/
Additional information of El Mondo:
Find more information/studies on trans fat, breast cancer and colorectal cancer right here.
A diet high in trans fat is a diet with more than 1 En% trans fat.
Trans fat can be found in doughnuts, cakes, pie crusts, biscuits, frozen pizza, cookies, crackers and stick margarines and other spreads.