Objectives:
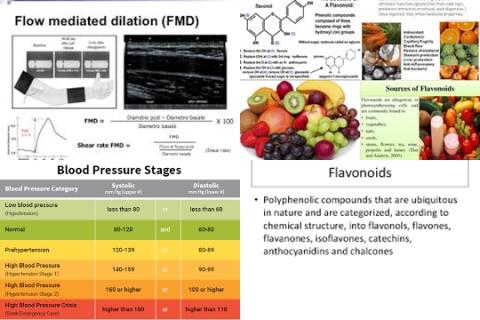
Does a low salt intake reduce blood pressure?
Study design:
This review article included 34 randomized trials with 3230 participants (the median age was 50 (range 22-73)), of which 22 were in hypertensive individuals and 12 in normotensive individuals. Of the 34 trials, 23 used crossover design and 11 used paralleled comparisons. 22 of the 34 trials were double blind, in 11 the observer was blind to blood pressure and one did not report any blinding procedure.
The study duration varied from 4 weeks to 3 years (median 4 weeks). With the usual salt intake the median 24 hour urinary sodium was 160 mmol (range 125-200 mmol), equivalent to a salt intake of 9.4 g/day (range 7.3-11.7 g/day) and the median blood pressure was 141/86 mmHg.
Despite the fact that only 7 out of 34 trials performed intention to treat analysis, the percentage of participants lost to follow-up after randomization was small (6.7% on average).
Results and conclusions:
The investigators found meta-analysis showed that the mean change in urinary sodium (reduced salt v usual salt) was -75 mmol/24 h (equivalent to a reduction of 4.4 g/day salt), and with this reduction in salt intake, the mean change in blood pressure was -4.18 mmHg [95% CI = -5.18 to -3.18, I2 = 75%] for systolic blood pressure and -2.06 mmHg [95% CI = -2.67 to -1.45, I2 = 68%] for diastolic blood pressure.
The investigators found meta-regression showed that age, ethnic group, blood pressure status (hypertensive or normotensive) and the change in 24 hour urinary sodium were all significantly associated with the fall in systolic blood pressure, explaining 68% of the variance between studies.
The investigators found a 100 mmol reduction in 24 hour urinary sodium (equivalent to a reduction 6 g/day salt) was associated with a fall in systolic blood pressure of 5.8 mmHg [95% CI = -2.5 to -9.2, p = 0.001] after adjustment for age, ethnic group and blood pressure status.
For diastolic blood pressure, age, ethnic group, blood pressure status and the change in 24 hour urinary sodium explained 41% of the variance between studies.
The investigators found meta-analysis by subgroup showed that in people with hypertension the mean effect was -5.39 mmHg [95% CI = -6.62 to -4.15, I2 = 61%] for systolic blood pressure and -2.82 mmHg [95% CI = -3.54 to -2.11, I2 = 52%] for diastolic blood pressure.
In normotensive people, the figures were -2.42 mmHg [95% CI = -3.56 to -1.29, I2 = 66%] and -1.00 mmHg [95% CI = -1.85 to -0.15, I2 = 66%], respectively.
The investigators found further subgroup analysis showed that the decrease in systolic blood pressure was significant in both white and black people and in men and women.
The investigators found meta-analysis of data on hormones and lipids showed that the mean change was:
0.26 ng/mL/h [95% CI = 0.17 to 0.36, I2 = 70%] for plasma renin activity;
73.20 pmol/L [95% CI = 44.92 to 101.48, I2 = 62%] for aldosterone;
187 pmol/L [95% CI = 39 to 336, I2 = 5%] for noradrenaline (norepinephrine);
37 pmol/L [95% CI = -1 to 74, I2 = 12%] for adrenaline (epinephrine);
0.05 mmol/L [95% CI = -0.02 to 0.11, I2 = 0%] for total cholesterol;
0.05 mmol/L [95% CI = -0.01 to 0.12, I2 = 0%] for low density lipoprotein cholesterol (LDL-cholesterol or bad cholesterol);
-0.02 mmol/L [95% CI = -0.06 to 0.01, I2 = 16%] high density lipoprotein cholesterol (HDL-cholesterol or good cholesterol) and:
0.04 mmol/L [95% CI = -0.02 to 0.09, I2 = 0%] for triglycerides.
The investigators concluded a modest reduction in salt intake of 4.4 g/day for 4 or more weeks causes, from a population viewpoint, important falls in blood pressure in people with both raised and normal blood pressure.
Salt reduction is associated with a small physiological increase in plasma renin activity, aldosterone and noradrenaline and no significant change in lipid concentrations.
The current recommendations to reduce salt intake from 9-12 to 5-6 g/day will have a major effect on blood pressure, but a further reduction to 3 g/day will have a greater effect and should become the long term target for population salt intake.
Original title:
Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials by He FJ, Li J and MacGregor GA.
Link:
http://www.bmj.com/content/346/bmj.f1325
Additional information of El Mondo:
Find more studies/information on sodium intake and hypertension right here.
A daily diet with a maximum of 3 grams salt per day is a diet with a maximum of 0.15 gram salt per 100 kcal.
A daily diet with a maximum of 0.15 gram salt per 100 kcal is a diet with mainly products/meals with a maximum of 0.15 gram salt per 100 kcal.