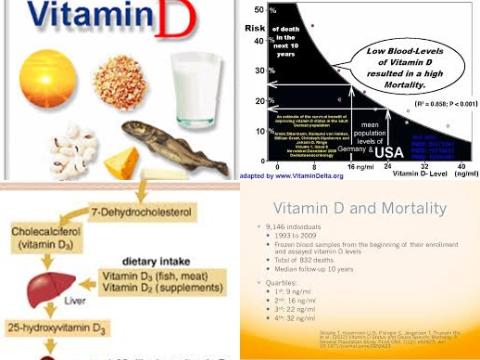
75-87.5 nmol/L vitamin D decrease mortality in the general population
Objectives:
Is there a relationship between serum 25(OH)D (vitamin D blood level) and mortality risk in the general population?
Study design:
This review article included 14 prospective cohort studies that involved 5562 deaths out of 62548 individuals.
In the parametric model, which is based on 11 studies and 59231 individuals, the lowest quantile as the reference category has been used.
Evidence of heterogeneity for the RR was apparent when highest were compared with lowest categories [p = 0.008, I2 = 58%].
There was no evidence of publication bias.
Results and conclusions:
The investigators found for “highest compared with lowest” categories of 25(OH)D, a significant reduced risk of 29% for mortality [RR = 0.71, 95% CI = 0.50-0.91].
The investigators found in the parametric model, the estimated summary RRs of mortality were 0.86 [95% CI = 0.82-0.91], 0.77 [95% CI = 0.70-0.84] and 0.69 [95% CI = 0.60-0.78] for individuals with an increase of 12.5, 25 and 50 nmol 25(OH)D serum values/L, respectively, from a median reference category of ∼27.5 nmol/L.
However, no significant decrease in mortality was found above ∼87.5 nmol/L.
The investigators concluded there is a nonlinear decrease in mortality risk as circulating 25(OH)D increases, with optimal concentrations ∼75-87.5 nmol/L. Because many adults do not achieve these 25(OH)D values, large prospective randomized trials are urgently needed to investigate whether vitamin D supplementation is able to reduce mortality risk in the general population.
Original title:
Vitamin D deficiency and mortality risk in the general population: a meta-analysis of prospective cohort studies by Zittermann A, Iodice S, [...], Gandini S.
Link:
http://ajcn.nutrition.org/content/95/1/91.full
Additional information of El Mondo:
Find more information/studies on vitamin D right here.