Objectives:
Although epidemiological studies have examined the role of chocolate in preventing cardiometabolic disease, the results remain inconsistent. Therefore, this review article (meta-analysis) has been conducted.
Does chocolate consumption reduce risk of coronary heart disease (CHD), stroke and diabetes?
Study design:
This review article included 14 prospective cohort studies, with 508,705 participants from six countries and 7,267 coronary heart disease (CHD) cases, 8,197 stroke cases and 13,271 diabetes cases.
The follow-up duration of the studies ranged from 5 to 16 years.
One serving was defined as 30g of chocolate.
The majority of chocolate consumed in the included studies was milk or dark chocolate.
Results and conclusions:
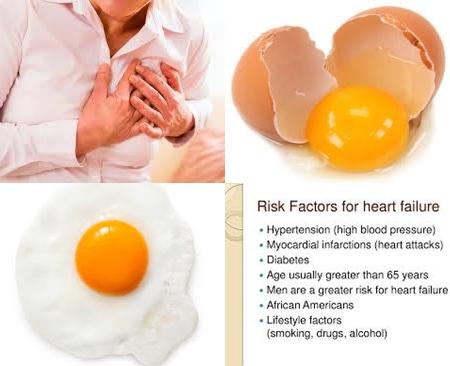
The investigators found in 6 cohort studies for the highest versus lowest intake of chocolate a significant reduced risk of 10% for coronary heart disease [pooled RR = 0.90, 95% CI = 0.82-0.97, I2 = 24.3%, p = 0.25]. Leave-one-out sensitivity analysis had no significant influence on the pooled results.
The investigators found regarding CHD subtype, a significant reduced risk of 14% [RR = 0.86, 95% CI = 0.77-0.96] for myocardial infarction.
The investigators found for studies with follow-up duration of 10 years a significant reduced risk of 28% for coronary heart disease [RR = 0.72, 95% CI = 0.57-0.92].
The investigators found for studies with follow-up duration of ≥10 years a significant reduced risk of 8% for coronary heart disease [RR = 0.92, 95% CI = 0.86-0.99].
The investigators found in dose-response meta-analysis of 5 studies a curvilinear association between chocolate consumption and risk of coronary heart disease [p for nonlinearity = 0.006].
The investigators found in dose-response meta-analysis, compared with no intake, a significant reduced risk of 6% for coronary heart disease for 1 serving (30g) chocolate per week [RR = 0.94, 95 CI = 0.90-0.99].
The investigators found in dose-response meta-analysis, compared with no intake, a significant reduced risk of 9% for coronary heart disease for 3 servings (90g) chocolate per week [RR = 0.91, 95 CI = 0.85-0.97].
The investigators found in dose-response meta-analysis, compared with no intake, a significant reduced risk of 11% for coronary heart disease for 7 servings (210g) chocolate per week [RR = 0.89, 95 CI = 0.83-0.95].
The investigators found in dose-response meta-analysis, compared with no intake, a significant reduced risk of 12% for coronary heart disease for 10 servings (300g) chocolate per week [RR = 0.88, 95 CI = 0.81-0.95].
The investigators found in 8 reports from 7 studies for the highest versus lowest level of chocolate consumption a significant reduced risk of 16% for stroke [pooled RR = 0.84, 95% CI = 0.78-0.90, I2 = 0%, p = 0.49]. The pooled risk of total stroke was not obviously modified in the sensitivity analysis by excluding one study at a time
Egger’s test suggested the presence of publication bias [p = 0.008]. However, after introducing the “trim and fill” method to adjust this bias, the overall risk estimate remained significant in favor of chocolate intake [RR = 0.86, 95% CI = 0.79-0.92].
The investigators found with regard to stroke subtypes, a significant reduced risk of 13% [RR = 0.87, 95% CI = 0.78-0.96] for cerebral infarction and a significant reduced risk of 17% [RR = 0.83, 95% CI = 0.71-0.97] for hemorrhagic stroke.
The investigators found in the stratified analysis by gender, a significant reduced risk of 13% of total stroke for male [RR = 0.87, 95% CI = 0.79-0.97] and a significant reduced risk of 16% of total stroke for female [RR = 0.84, 95% CI = 0.74-0.94].
The investigators found a significant reduced risk of 44% for studies with follow-up durations of 10 years [RR = 0.56, 95% CI = 0.37-0.85].
The investigators found a significant reduced risk of 15% for studies with follow-up durations of ≥10 years [RR = 0.85, 95% CI = 0.79-0.91].
The investigators found in 7 reports from 6 studies a nonlinear correlation between chocolate intake and risk of stroke [p for nonlinearity = 0.001].
The investigators found in dose-response meta-analysis, compared with no intake, a significant reduced risk of 9% for stroke for 1 serving chocolate per week [RR = 0.91, 95% CI = 0.86-0.97].
The investigators found in dose-response meta-analysis, compared with no intake, a significant reduced risk of 13% for stroke for 3 servings chocolate per week [RR = 0.87, 95% CI = 0.81-0.94].
The investigators found in dose-response meta-analysis, compared with no intake, a significant reduced risk of 15% for stroke for 7 servings chocolate per week [RR = 0.85, 95% CI = 0.76-0.93].
The investigators found in dose-response meta-analysis, compared with no intake, a significant reduced risk of 17% for stroke for 10 servings chocolate per week [RR = 0.83, 95% CI = 0.72-0.94].
The investigators found in 4 studies using “trim and fill” method, for the highest versus lowest intake of chocolate, a non-significant reduced risk of 8% for diabetes [pooled RR = 0.92, 95% CI = 0.78-1.08].
The investigators found in stratified analysis by sex, a significant reduced risk of 21% [RR = 0.79, 95% CI = 0.65-0.96] for men and a non-significant reduced risk of 8% [RR = 0.92, 95% CI = 0.72-1.17] for women.
Similarly, the risks of diabetes were not different between subsets of studies with follow-up durations of below or over 10 years [p for interaction = 0.51].
The investigators found in dose-response meta-analysis of 6 reports, a curvilinear association between chocolate intake and risk of diabetes [p for nonlinearity 0.001].
The investigators found in dose-response meta-analysis, compared with no intake, a significant reduced risk of 20% for diabetes for 1 serving chocolate per week [RR = 0.80, 95% CI = 0.71-0.91]. Significant means that there is an association with a 95% confidence.
The investigators found in dose-response meta-analysis, compared with no intake, a significant reduced risk of 24% for diabetes for 3 servings chocolate per week [RR = 0.76, 95% CI = 0.63-0.91]. Significant because RR of 1 was not found in the 95% CI of 0.63 to 0.91. RR of 1 means no risk/association.
The investigators found in dose-response meta-analysis, compared with no intake, a non-significant reduced risk of 17% for diabetes for 7 servings chocolate per week [RR = 0.83, 95% CI = 0.67-1.03]. Non-significant means it cannot be said with a 95% confidence that 7 servings chocolate per week really decreased the risk of diabetes with 17%.
The investigators found in dose-response meta-analysis, compared with no intake, a non-significant reduced risk of 11% for diabetes for 10 servings chocolate per week [RR = 0.89, 95% CI = 0.69-1.16].
The investigators found in general, the dose-response pattern was J-shaped and the peak reduction in diabetes risk occurred at an intake of 2 servings/week [RR = 0.75, 95% CI = 0.63-0.89], with no protective effects observed when consuming chocolate > 6 servings/week.
The investigators concluded that chocolate consumption confers reduced risks of coronary heart disease, stroke and diabetes. Consuming chocolate in moderation (1-6 servings/week or 30-180g) may be optimal for the prevention of these burdensome diseases. However, additional large prospective studies are required to confirm the observed benefits of chocolate in populations with different characteristics and to establish the optimum frequency of chocolate intake for preventing cardiometabolic disease.
Original title:
Chocolate Consumption and Risk of Coronary Heart Disease, Stroke, and Diabetes: A Meta-Analysis of Prospective Studies by Yuan S, Li X, […], Lu J.
Link:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5537803/
Additional information of El Mondo:
Find more information/studies on chocolate, diabetes and cardiovascular diseases right here.