Flavonoid supplements show significant improvements in vascular function and blood pressure
Objectives:
Previous systematic reviews suggest beneficial effects of flavonoids on biomarkers of cardiovascular disease (CVD) risk, but have overlooked the impact of dose response or food complexity. Therefore, this review article has been conducted.
Do taking flavonoid supplements improve flow-mediated dilation (FMD) and blood pressure?
Study design:
This review article included 63 RCTs.
Results and conclusions:
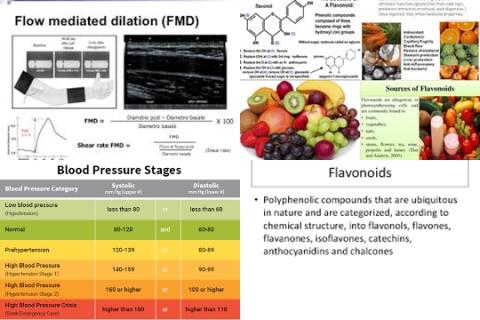
The investigators found meta-analyses of combined flavonoid subclasses showed significant improvements in FMD [chronic: 0.73%, 95% CI = 0.17 to 1.30, 14 RCTs and acute: 2.33%, 95% CI = 1.58 to 3.08, 18 RCTs].
The investigators found meta-analyses of combined flavonoid subclasses showed significant improvements in blood pressures [systolic: -1.46 mmHg, 95% CI = -0.38 to -0.53, 63 RCTs and diastolic: -1.25 mmHg, 95% CI = -1.82 to -0.67, 63 RCTs].
The investigators found similar benefits were observed for the flavan-3-ol, catechol flavonoids (catechins, quercetin, cyanidin etc.), procyanidins, epicatechin and catechin subgroups.
The investigators found dose-response relationships were non-linear for FMD (R2 ≤ 0.30), with greater associations observed when applying polynomial regression analyses (R2 ≤ 0.72). However, there was no indication of a dose response for blood pressure.
The investigators concluded flavonoid subclasses supplements show significant improvements in FMD and blood pressure. However, the flavonoid bioactivity does not follow a classical linear dose-response association and this may have important biological implications.
Original title:
Relative impact of flavonoid composition, dose and structure on vascular function: A systematic review of randomised controlled trials of flavonoid-rich food products by Kay CD, Hooper L, […], Cassidy A.
Link:
http://onlinelibrary.wiley.com/doi/10.1002/mnfr.201200363/abstract;jsessionid=2CCB9E4E779A221E42AA38998C865DA6.d02t03?deniedAccessCustomisedMessage=&userIsAuthenticated=false
Additional information of El Mondo:
Find more information/studies on RCTs, lowering blood pressure and cardiovascular disease right here.
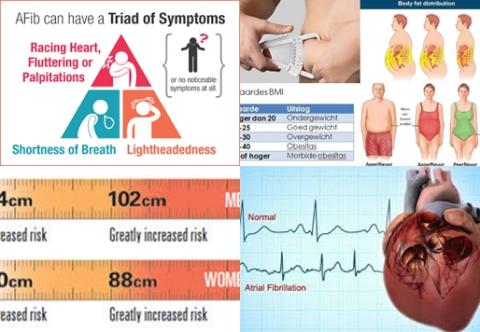
The optimal blood pressure for a healthy adult is120 mmHg systolic pressure and 80 mmHg diastolic pressure.
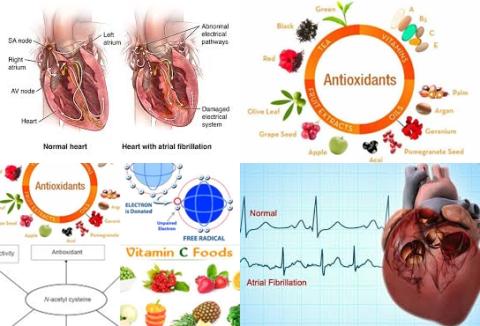
When blood flow increases through a vessel, the vessel dilates. This phenomenon has been coined flow-mediated dilatation (FMD). Flow-mediated dilation is an accepted technique to quantify endothelial function and has shown to have prognostic value for future cardiovascular disease (CVD).