Zinc supplementation does not increase brain derived neurotrophic factor levels
Objectives:
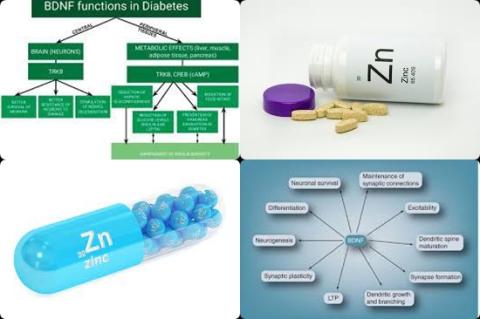
Zinc in one of the most abundant trace minerals in human body which is involved in numerous biological pathways and has variety of roles in the nervous system. It has been assumed that zinc exerts its role in nervous system through increasing brain derived neurotrophic factor (BDNF) concentrations. Therefore, this review article has been conducted.
Does zinc supplementation increase brain derived neurotrophic factor (BDNF) levels?
Study design:
This review article included 5 studies with 238 participants. These studies enrolled subjects with premenstrual syndrome, diabetic retinopathy, major depression disorder, overweight/obese and obese with mild to moderate depressive disorders.
Funnel plot did not suggest publication bias.
Results and conclusions:
The investigators found zinc supplementation failed to increase blood brain derived neurotrophic factor concentrations with effect size of 0.30 [95% CI = -0.08 to 0.67, p = 0.119].
The investigators concluded zinc supplementation does not increase brain derived neurotrophic factor (BDNF) levels. However, the small number of included articles and significant heterogeneity between them can increase the risk of a false negative result; therefore, the results should be interpreted with caution.
Original title:
The effect of zinc supplementation on brain derived neurotrophic factor: A meta-analysis by Jafari F, Mohammadi H and Amani R.
Link:
https://pubmed.ncbi.nlm.nih.gov/33831797/
Additional information of El Mondo:
Find here more information/studies about review article/significant and zinc.
Brain Derived Neurotrophic Factor (BDNF) plays an important role in neuronal survival and growth, serves as a neurotransmitter modulator and participates in neuronal plasticity, which is essential for learning and memory.
Decreased levels of BDNF are associated with neurodegenerative diseases with neuronal loss, such as Parkinson's disease, Alzheimer's disease, multiple sclerosis and Huntington's disease.