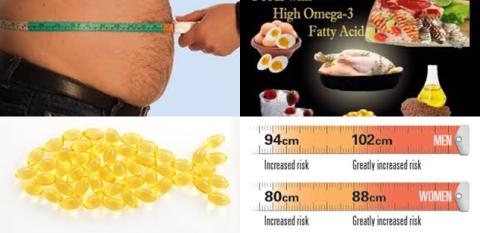
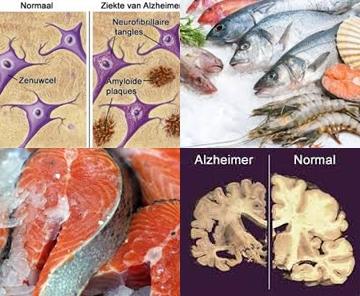
Fish oil supplementation during <12 weeks improves insulin sensitivity among people with metabolic disorders
Objectives:
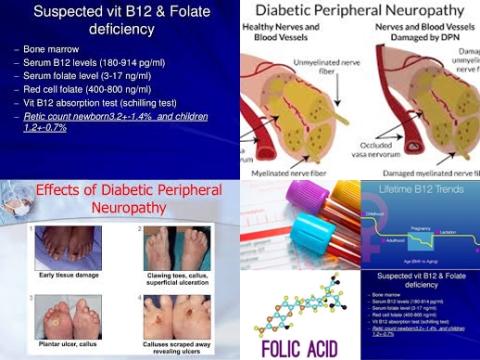
Fish oil supplementation has been shown to be associated with a lower risk of metabolic syndrome and benefit a wide range of chronic diseases, such as cardiovascular disease, type 2 diabetes and several types of cancers. However, the evidence of fish oil supplementation on glucose metabolism and insulin sensitivity is still controversial. Therefore, this review article (meta-analysis) has been conducted.
Does fish oil supplementation improve insulin sensitivity in humans?
Study design:
This review article included a total of 17 RCTs with 672 participants. One of the 17 studies was crossover design and others were parallel design.
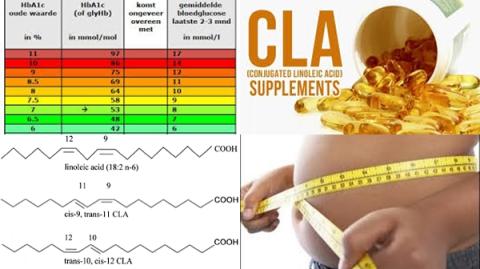
The doses of active ingredients of fish oil (n-3 fatty acids) ranged from 1 g/d to 4 g/d. Duration of the interventions was ranged from 4 weeks to 24 weeks.
There was no suggestion of small study effect based on visual inspection of the funnel plot. Results of the Egger’s (p = 0.78) and Begg’s (p = 0.43) tests showed that there was no potential publication bias.
Results and conclusions:
The investigators found pooled analysis showed that fish oil supplementation had no effects on insulin sensitivity overall [SMD = 0.17, 95% CI = -0.15 to 0.48, p = 0.292, I2 = 58.1%, p = 0.001].
The investigators found subgroup analysis showed that fish oil supplementation significantly improved insulin sensitivity among people who were experiencing at least one symptom of metabolic disorders [SMD = 0.53, 95% CI = 0.17 to 0.88, p 0.001].
The investigators found subgroup analysis showed a positive effect of fish oil on insulin sensitivity among the short-term intervention group (12 weeks) rather than the long-term intervention group [SMD = 0.31, 95% CI = 0.01-0.61, p = 0.04].
The investigators found subgroup analysis showed that fish oil had no effects on insulin sensitivity among the healthy people or people with T2DM.
The investigators found there were no significant differences between subgroups of methods of insulin sensitivity and doses of omega-3 polyunsaturated fatty acids (n-3 PUFA) of fish oil supplementation.
The investigators found in sensitivity analysis that summary results did not differ significantly when omitting studies one at a time.
The investigators concluded that fish oil supplementation during 12 weeks improves insulin sensitivity among people who were experiencing at least one symptom of metabolic disorders.
Original title:
Fish oil supplementation and insulin sensitivity: a systematic review and meta-analysis by Gao H, Geng T, [...], Zhao Q.
Link:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5496233/
Additional information of El Mondo:
Find more information/studies on fish oil supplements and diabetes right here.