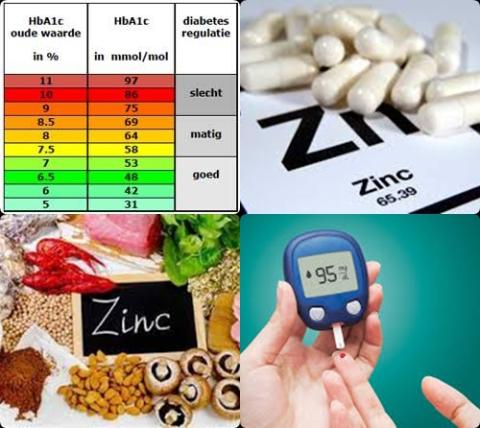
Elevated serum/plasma zinc concentration increases risk of type 2 diabetes

Objectives:
The role of zinc in the etiology of type 2 diabetes has been widely reported in recent decades. However, much remains uncertain concerning the effect of zinc on the risk of developing type 2 diabetes. Therefore, this review article has been conducted.
Does zinc reduce risk of type 2 diabetes?
Study design:
This review article included 16 studies.
There was no publication bias.
Results and conclusions:
The investigators found in 7 prospective cohort studies and 1 cross-sectional study (146,027 participants aged between 18 and 84 years and of both genders, belonging to different ethnic groups. Of which, 11,511 type 2 diabetes cases) when comparing the highest versus lowest dietary zinc intakes, a significantly reduced risk of 13% [OR = 0.87, 95% CI = 0.78-0.98, I2 = 64.5%, p = 0.003] for type 2 diabetes.
This relationship was stronger and more evident in rural compared to urban areas [rural areas: OR = 0.59, 95% CI = 0.48-0.73, I2 = 0.0%, p = 0.843 versus urban areas: OR = 0.94, 95% CI = 0.86-1.02, I2 = 43.9%, p = 0.113].
The investigators found no association between supplementary [OR = 0.94, 95% CI = 0.75-1.19, I2 = 85.4%, p = 0.009] or total zinc intake from both diet and supplementation [OR = 0.95, 95% CI = 0.82-1.11, I2 = 56.5%, p = 0.129] and type 2 diabetes risk.
The investigators found in population-based studies that high serum/plasma zinc levels significantly increased risk of type 2 diabetes with 64% [OR = 1.64, 95% CI = 1.25-2.14, I2 > 22.5%, p = 0.275].
The investigators concluded high dietary zinc intake reduces risk of type 2 diabetes. This relationship is stronger and more evident in rural compared to urban areas. However, an elevated serum/plasma zinc concentration is associated with an increased risk of type 2 diabetes in the general population.
Link:
Zinc Intake and Status and Risk of Type 2 Diabetes Mellitus: A Systematic Review and Meta-Analysis by Fernández-Cao JC, Warthon-Medina M, […], Lowe NM.
Link:
https://www.mdpi.com/2072-6643/11/5/1027/htm
Additional information of El Mondo:
Find more information/studies on diabetes and zinc consumption right here.
Serum/plasma zinc levels can be increased by eating products that contain a lot of zinc and/or taking zinc supplements.