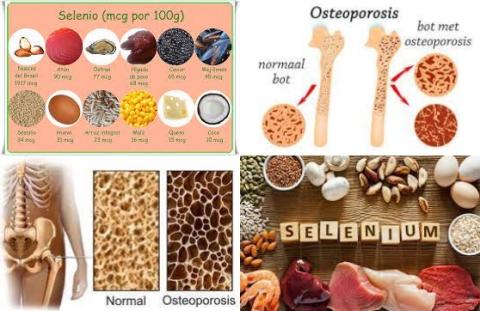
High selenium dietary intake reduces hip fracture
Objectives:
Previous studies have suggested that selenium as a trace element is involved in bone health, but findings related to the specific effect of selenium on bone health remain inconclusive. Therefore, this review article has been conducted.
Do both high dietary selenium intake and high serum selenium levels increase bone density?
Study design:
This review article included 8 cross-sectional studies, 7 case-control studies and 3 prospective cohort studies and 1 RCT with a total of 69,672 subjects.
The number of participants ranged from 60 to 21,939, while the mean age varied from 39.4 to 75.8 years, with mean selenium intake ranging from 41.2 to 154.4 μg/d or mean serum selenium level ranging from 66.7 to 131.1 μg/L.
All the observational studies had a NOS score ≥ 4, namely moderate- to high-quality scores.
There was no publication bias.
Results and conclusions:
The investigators found a significantly positive association between dietary selenium intake [β = 0.04, 95% CI = 0.00 to 0.07, p = 0.029, I2 = 95.91%] as well as serum selenium [β = 0.13, 95% CI = 0.00 to 0.26, p = 0.046, I2 = 86.60%] and bone mineral density.
The investigators found high dietary selenium intake significantly reduced risk of hip fracture with 56% [OR = 0.44, 95% CI = 0.37 to 0.52, p 0.001, I2 = 65.2%].
The investigators found osteoporosis patients had lower serum selenium level than healthy controls [WMD = -2.01, 95% CI = -3.91 to -0.12, p = 0.037, I2 = 0%].
The investigators concluded persons with higher dietary selenium intake and higher serum selenium have higher bone mineral density. Furthermore, high selenium dietary intake reduces hip fracture.
Original title:
The association between selenium and bone health: a meta-analysis by Xie H, Wang N, […], Wang Y.
Link:
https://boneandjoint.org.uk/article/10.1302/2046-3758.127.BJR-2022-0420.R1
Additional information of El Mondo:
Find more information/studies on selenium and preventing fractures right here.
Circulating concentration of selenium in blood (serum selenium level) can be increased by eating foods that are high in selenium and/or taking selenium supplements.