EPA + DHA supplements for at least 6 months increase walking speed among the elderly

Objectives:
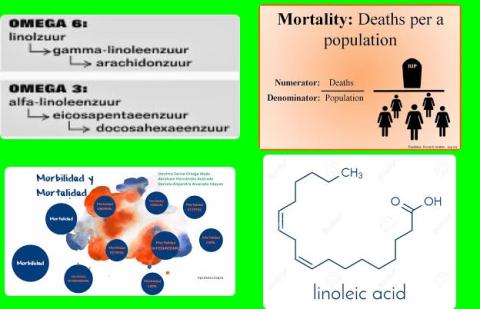
Do omega-3 fatty acid supplements (EPA and DHA) improve sarcopenia-related performances among the elderly?
Study design:
This review article included 10 RCTs with 552 participants.
The number of study participants ranged from 24 to 126 and the durations of the interventions spanned 10 to 24 weeks.
The doses ranged from 0.16 to 2.6 g/day of EPA and from 0 to 1.8 g/day of DHA.
The mean ages of the participants across the RCTs ranged from 63 to 75 years old.
Results and conclusions:
The investigators found in subgroup analyses that omega-3 fatty acid supplements (EPA and DHA) at more than 2 g/day significantly increased muscle mass among the elderly [SMD = 0.67 kg, 95% CI = 0.16 to 1.18, p 0.05].
The investigators found in subgroup analyses that omega-3 fatty acid supplements (EPA and DHA) during more than 6 months significantly improved walking speed among the elderly [SMD = 1.78 m/sec, 95% CI = 1.38 to 2.17, p 0.05].
The investigators concluded that taking at least 2 grams of omega-3 supplements (EPA and DHA) per day increases muscle mass among the elderly, while taking omega-3 supplements for at least 6 months increases walking speed among the elderly.
Original title:
Effects of Omega-3 Fatty Acids on Muscle Mass, Muscle Strength and Muscle Performance among the Elderly: A Meta-Analysis by Huang YH, Chiu WC, […], Wang YH.
Link:
https://www.mdpi.com/2072-6643/12/12/3739/htm
Additional information of El Mondo:
Find more information/studies on EPA and DHA consumption and elderly right here.
EPA and DHA are present in fish.