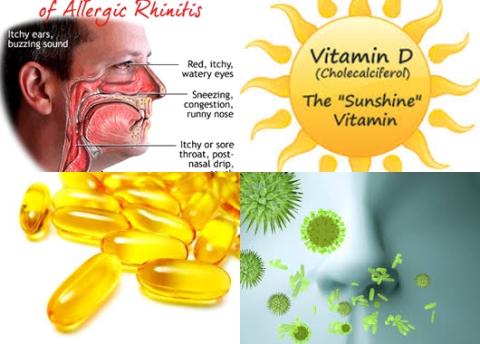
Daily 200-320 micrograms dietary folate intake reduce breast cancer risk
Objectives:
Previous observational studies regarding the existence of an association between folate intake and the risk of breast cancer have been inconsistent. Therefore, this review article has been conducted.
Does a higher dietary folate intake reduce breast cancer risk?
Study design:
This review article included 14 prospective cohort studies that reported data on 677,858 individuals.
The participant follow-up period ranged 4.7-17.4 years and the number of individuals per study ranged 11,699-88,818.
There was no publication bias.
Results and conclusions:
The investigators found no association between dietary folate intake and breast cancer risk for highest versus lowest category [RR = 0.97, 95% CI = 0.90-1.05, p = 0.451, I2 = 57.5%, p = 0.004].
The investigators found dose-response meta-analysis findings showed no association between the risk of breast cancer and a 100 µg/day increase in dietary folate intake [RR = 0.99, 95% CI = 0.98-1.01, p = 0.361, I2 = 66.2%, p 0.001].
The investigators found evidence of a nonlinear relationship between dietary folate intake and the risk of breast cancer.
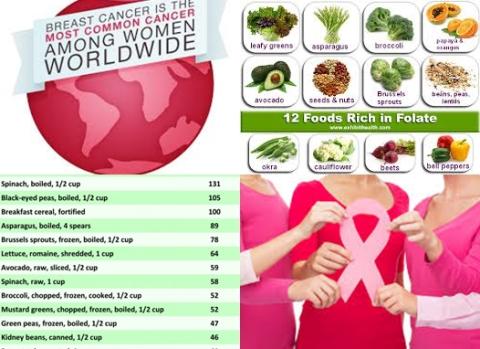
A daily dietary folate intake of 200-320 µg was associated with a reduced risk of breast cancer. However, daily folate intake levels >400 µg was associated with a increased risk of breast cancer.
The investigators found overall folate intake level was associated with a reduced breast cancer risk of 36% if the patients had a daily alcohol intake >10 g [RR for highest versus lowest category = 0.64, 95% CI = 0.43-0.97].
The investigators concluded there are no effects of increased dietary folate intake on the incidence of breast cancer. But, a daily dietary folate intake of 200-320 µg was associated with a reduced risk of breast cancer. However, daily folate intake levels >400 µg was associated with a increased risk of breast cancer. Future studies should focus on specific populations in order to analyze primary breast cancer prevention.
Original title:
Folate Intake and the Risk of Breast Cancer: A Dose-Response Meta-Analysis of Prospective Studies by Zhang YF, Shi WW, […], Zhou YH.
Link:
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4059748/
Additional information of El Mondo:
Find more studies/information on folate intake and breast cancer right here.