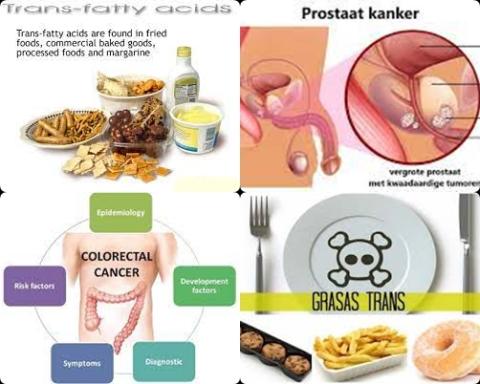
Obesity increases colorectal cancer in men with Lynch Syndrome

Objectives:
There appears to be a sex-specific association between obesity and colorectal neoplasia in patients with Lynch Syndrome (LS). Therefore, this review article has been conducted.
Does obesity (BMI>30) increase colorectal cancer in patients with Lynch Syndrome?
Study design:
This review article included 3 prospective cohort studies with 2,463 subjects (persons), of which 735 subjects with colorectal cancer.
All studies with a prospective study design (cohort studies) expressed the association between obesity and colorectal cancer in terms of adjusted HR (95% CI).
There was no publication bias.
Results and conclusions:
The investigators found a twofold risk of colorectal cancer in obese men with Lynch Syndrome compared to nonobese men with Lynch Syndrome [SRR = 2.09, 95% CI = 1.23 to 3.55, I2 = 33%].
No significantly increased risk due to obesity was found for women [SRR = 1.41, 95% CI = 0.46 to 4.27, I2 = 68%].
The investigators found a significantly 49% increased colorectal cancer risk for obesity (BMI>30) for subjects with an MLH1 mutation [SRR = 1.49, 95% CI = 1.11 to 1.99, I2 = 0%].
The investigators concluded that obesity (BMI>30) increases colorectal cancer in men with Lynch Syndrome, particularly with an MLH1 mutation.
Original title:
A Meta-Analysis of Obesity and Risk of Colorectal Cancer in Patients with Lynch Syndrome: The Impact of Sex and Genetics by Lazzeroni M, Bellerba F, […], Gandini S.
Link:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8160758
Additional information of El Mondo:
Find more information/studies on cancer and obesity/overweight right here.
Lynch syndrome, also known as hereditary non-polyposis colorectal cancer (HNPCC), is an autosomal dominantly inherited disease. People with Lynch syndrome have about a 40% to 80% chance of getting colorectal cancer by age 70. They’re also at risk for cancer of the uterus, ovaries or stomach. And they tend to get cancer at younger ages than other people, often in their 30s and 40s.
An error or mutation, in one copy of the MLH1 gene is one of the causes of Lynch syndrome. Men and women with a mutation in MLH1 have a 52-82% lifetime risk (up to age 70) to develop colon or rectal cancer.