Objectives:
The relationship between intake of fish and n-3 fatty acids and endometrial cancer risk has not been consistent across epidemiological studies. Therefore, this review article (meta-analysis) has been conducted.
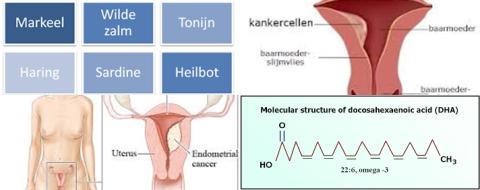
Do fish consumption and dietary EPA and DHA intake reduce endometrial cancer risk?
Study design:
This review article included 4 prospective cohort studies, 1 case-cohort study and 11 case-control studies (including 8 population-based case-control studies and 3 hospital-based case-control studies).
The prospective cohort studies had a mean follow-up of 6.5 to 9.1 years.
The highest category of fish ranged from >1-2 servings/week to >15.4 servings/week,
The highest category of DHA ranged from 143 to 227 mg/d.
The highest category of EPA ranged from 74.7 to 127 mg/d.
When fish intake was reported in unit of g/d, it was converted to serving/week by assuming 1 serving = 100g.
Overall, all 16 studies were classified as high-quality studies.
There was no publication bias.
Results and conclusions:
The investigators found a non-significant association between the highest vs. lowest category of fish consumption and endometrial cancer risk [RR = 1.04, 95% CI = 0.84-1.30, I2 = 80.4%].
According to the subgroup analyses, the null association persisted in strata according to study design, location, type of controls, number of cases, publication year and adjustments of energy intake, reproductive factors and smoking.
The investigators found in subgroup analyses for every one additional serving/week of fish intake, a significant reduced risk of 10% for endometrial cancer in studies conducted in Europe [RR = 0.90, 95% CI = 0.84-0.97]. Significant means that there is an association with a 95% confidence.
The investigators found in subgroup analyses for every one additional serving/week of fish intake, a significant increased risk of 15% for endometrial cancer in studies conducted in Asia [RR = 1.15, 95% CI = 1.10-1.21]. Significant because RR of 1 was not found in the 95% CI of 1.10 to 1.21. RR of 1 means no risk/association.
The investigators found in studies adjusting for smoking for every one additional serving/week of fish intake, a significant reduced risk of 5% for endometrial cancer [RR = 0.95, 95% CI = 0.91-1.00].
The investigators found in studies without an adjustment of smoking for every one additional serving/week of fish intake, a significant increased risk of 14% for endometrial cancer [RR = 1.14, 95% CI = 1.09-1.19].
The investigators found a non-significant inverse association between the highest category of DHA intake and endometrial cancer risk [RR = 0.85, 95% CI = 0.64-1.11, I2 = 59.6%]. However, the dose-response analysis suggested a significant non-linear relationship between DHA intake and endometrial cancer risk [p = 0.04 and p for heterogeneity = 0.39], with a decreased risk being detected for an intake of DHA no more than 175 mg/d.
The investigators concluded that there is a significant inverse association between every one additional serving/week of fish intake and endometrial cancer risk in studies conducted in Europe and studies adjusted for smoking. Furthermore, there is a significant non-linear relationship between DHA intake and risk of endometrial cancer, with a decreased risk being detected for an intake of DHA no more than 175 mg/d. Further well-designed studies are warranted to better characterize the relationship between fish, n-3 PUFA and endometrial cancer development.
Original title:
Dietary n-3 polyunsaturated fatty acids, fish consumption, and endometrial cancer risk: a meta-analysis of epidemiological studies by Hou R, Yao SS, […], Jiang L.
Link:
http://www.impactjournals.com/oncotarget/index.php?journal=oncotarget&page=article&op=view&path[]=18295&path[]=58664
Additional information of El Mondo:
Find more information/studies on fish consumption, significant/cohort/95% CI and cancer right here.
These fish contain 175 mg DHA.