Diabetes
Scientific studies (review articles) on the relationship between diet/nutrients and diabetes prevention:
One swallow does not make a summer. A famous Dutch saying that could not be any more obvious. Just because one single scientific study about a certain topic makes certain claims, it does not necessarily mean it is true. On the other hand, a review article (a collection of scientific studies on a certain topic) of randomized, placebo-controlled double blind clinical trials (RCTs) will answer the following question:
"Do taking dietary supplements make sense?" Yes for a positive conclusion and no for a negative conclusion.
One swallow does not make a summer. A famous Dutch saying that could not be any more obvious. Just because one single scientific study about a certain topic makes certain claims, it does not necessarily mean it is true. On the other hand, a review article (a collection of scientific studies on a certain topic) of cohort studies or case-control studies will answer the following question:
"Should I change my diet?".
2024:
2022:
- 500 mg/d dietary flavonoid intake reduces cardiovascular disease, diabetes and hypertension
- Vitamin D deficiency increases blindness in people with diabetes
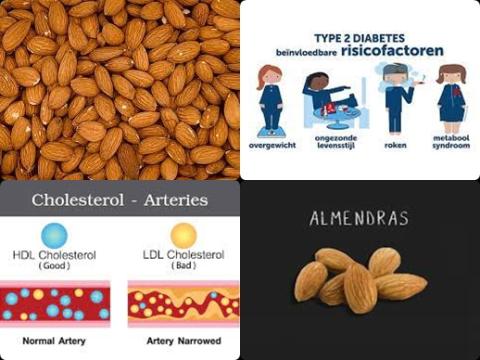
- 50 g/d almond decreases causally bad cholesterol in patients with type 2 diabetes
- Ginger supplementation reduces blood pressure in patients with type 2 diabetes
2021:
- Higher concentrations of carotenoids reduce type 2 diabetes
- Dietary sodium restriction causally reduces blood pressure in patients with type 2 diabetes mellitus
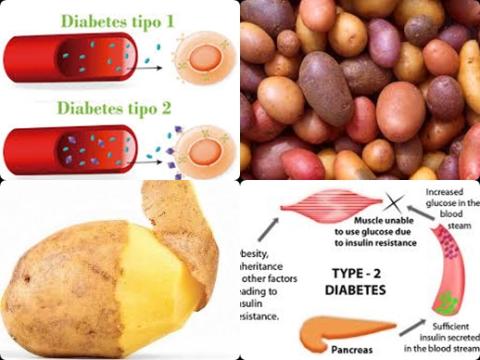
- Daily 80g potato increase type 2 diabetes among Western populations
- Vitamin C supplements improve triglyceride and cholesterol levels in patients with type 2 diabetes mellitus
- Spirulina supplementation reduces bad cholesterol among type 2 diabetes patients
- Grapes/grape products supplementation reduces HOMA-IR values in adults
- Intensive glucose control slows down cognitive decline in persons with type 2 diabetes
- Chromium supplementation improves lipid profile in patients with type 2 diabetes mellitus
- Patients with diabetes mellitus should be vaccinated against herpes zoster
- L-arginine supplements do not reduce diabetes in adults
- 1.5 g/day garlic supplementation reduces adiponectin level among participants ˂30 years
- Mortality is more frequently in COVID-19 patients with chronic kidney diseases and cardiovascular disease
- Peanut butter consumption may reduce type 2 diabetes
- Patients older than 60 years, with hypertension, diabetes and D-dimer values above 3.17 µg/mL have higher thrombotic events due to COVID-19
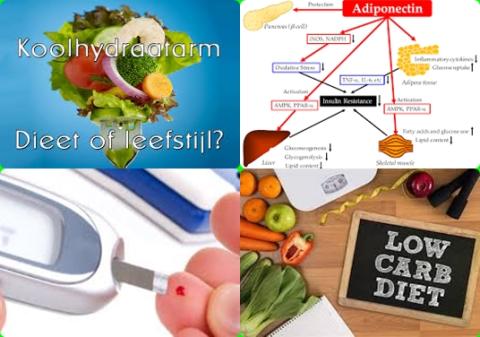
- Diet with <30 En% carbohydrates causally increases adiponectin concentration in adults
- 1.5 g/day EPA + DHA improve insulin sensitivity in children
- Oral vitamin C supplementation may improve glycemic control and blood pressure in people with type 2 diabetes
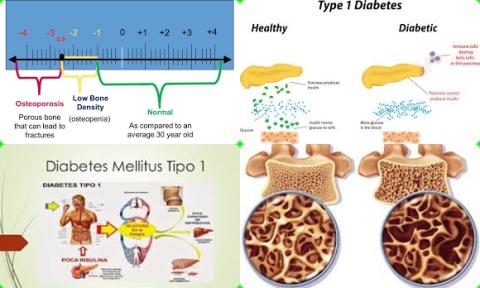
- Type 1 diabetes mellitus decreases bone mineral density in children and adolescents
2020:
- BCG vaccine should not be used in treatment of type 1 diabetes mellitus
- 2-3 servings/week fish reduce all-cause mortality in patients with type 2 diabetes
- Most prevalent comorbidities among COVID-19 are hypertension, diabetes, cardiovascular disease, liver disease, lung disease, malignancy, cerebrovascular disease, COPD and asthma
- Vitamin B3 supplementation increases good cholesterol in patients with type 2 diabetes mellitus
- Patients with diabetes should be advised to continue taking metformin drugs despite COVID-19 infection status
- Daily 8.4-10 grams of inulin supplements for at least 8 weeks improve risk factors of type 2 diabetes
- Male, age, cardiovascular disease, hypertension and diabetes mellitus increase mortality in patients with COVID-19
- Diabetes mellitus is associated with severe infection and mortality in patients with COVID-19
- Barberry supplementation improves insulin levels
- Diabetes increases in-hospital mortality in patients with COVID-19
- Daily 40g soy consumption for <12 weeks increase IGF-1 level
- 100 mg/day magnesium dietary intake reduce type 2 diabetes
- 50g/day processed meat increase type 2 diabetes
- Yogurt intake is associated with a reduced risk of type 2 diabetes
- Hypertension, diabetes, COPD, cardiovascular disease and cerebrovascular disease are major risk factors for patients with COVID-19
- Hypertension, cardiovascular diseases, diabetes mellitus, smoking, COPD, malignancy and chronic kidney disease are risk factors for COVID-19 infection
- Omega-3 fatty acids + vitamin E or D reduce gestational diabetes
- Psyllium consumption improves risk factors of diabetes
- Soy protein dietary intake reduces type 2 diabetes
2019:
- Elevated serum/plasma zinc concentration increases risk of type 2 diabetes
- 100mg magnesium dietary intake reduce type 2 diabetes
- Consumption of tree nuts decreases HOMA-IR and fasting insulin levels
- Low-fat dairy products have a beneficial effect on HOMA-IR, waist circumference and body weight
- Whole grain and cereal fiber dietary intake reduce type 2 diabetes
- Dietary low-ratio n-6/n-3 PUFA supplementation improves insulin resistance in diabetic patients
- Zinc supplementation reduces diabetes mellitus
- Moderate plant protein decreases type 2 diabetes mellitus
- Probiotic and synbiotic supplementation reduce inflammation in diabetic patients
- Folate supplementation lowers HOMA-IR
- 13.1 g/day viscous fiber supplements improve glycemic control
2018:
- 1 serving/day potato increases risk type 2 diabetes
- 150 g/day French-fries consumption increases risk of hypertension
- Garlic increases good cholesterol in diabetic patients
- High intake of cereal fiber may reduce type 2 diabetes
- Ginger intake reduces body weight and fasting glucose among overweight and obese subjects
- Animal protein increases risk of type 2 diabetes
- ≥550 mg/day flavonoids intake reduce type 2 diabetes
- High-fat diets increase risk of type 2 diabetes
- Folic acid supplementation reduces both fasting glucose level, fasting insulin level and HOMA-IR
- Low-GI diet is good for patients with type 2 diabetes
- Vitamin K supplementation has no effect on glycemic control
- Daily 3 mg L-carnitine during 12 weeks reduce serum leptin concentrations in diabetic patients
2017:
- Each 1 mmol/L increase in serum potassium reduces type 2 diabetes mellitus by 17%
- Fish oil supplementation during <12 weeks improves insulin sensitivity among people with metabolic disorders
- Atrial fibrillation, previous stroke, myocardial infarction, hypertension, diabetes and previous TIA increase risk of post-stroke dementia
- Pomegranate supplementation has no favourable effect on improvements in glucose and insulin metabolism
- Low carbohydrate diet decreases type 2 diabetes
- A diet with 4.4 g/day alpha-linolenic acid during 3 months does not reduce level of HbA1c, FBG or FBI in patients with type 2 diabetes
- Vegetarian diet has a protective effect against diabetes risk
- Weekly 30-180 gram chocolate consumption reduces risk of coronary heart disease, stroke and diabetes
- Probiotics supplementation improves HbA1c and fasting insulin in type 2 diabetes patients
- Vitamin K supplementation does not reduce diabetes
- A higher consumption of whole grains, fruits and dairy products reduces type 2 diabetes risk
- A diet of below 45 En% carbohydrate during 3 to 6 months reduces HbA1c level of patients with type 2 diabetes
- Vitamin C supplementation for at least 30 days reduces glucose concentrations in patients with type 2 diabetes
- Magnesium supplementation reduces risk of cardiovascular disease among type 2 diabetes
- Weekly one serving of apple and pear reduces type 2 diabetes mellitus risk
- Reduced serum levels of folate and vitamin B12 increase peripheral neuropathy risk among patients with type 2 diabetes
- Vitamin C and D reduce blood pressure in patients with type 2 diabetes
2016:
2015:
2014:
- Exercise lowers the risk for diabetes conferred by insulin resistance
- 1-6 cups/day caffeinated or decaffeinated coffee is associated with reduced type 2 diabetes risk
- Exercise training helps to prevent and to treat type 2 diabetes in youth
- At least 25g dietary fiber intake per day reduces risk of type 2 diabetes
- Niacin supplementation reduces LDL cholesterol levels in patients with type 2 diabetes mellitus
2012:
Diabetes increases risk of dementia and mild cognitive impairment
XXXXXXXXXX
The human body wants the blood glucose (blood sugar) level maintained in a very narrow range of 4 to 8 mmol/l. Insulin and glucagon are the hormones which make this happen. Both insulin and glucagon are secreted from the pancreas.
When the blood glucose level drops below 4 mmol/l (after physical exercise or on awakening) the alpha cells of the pancreas release glucagon. Glucagon converts glycogen into glucose. The glucose is released into the bloodstream, increasing blood sugar levels.
On the other hand, when the blood glucose level rises above 8 mmol/l, whether as a result of glycogen conversion or from digestion of a meal, insulin is released from beta cells of the pancreas. This hormone causes the liver to convert more glucose into glycogen and to force about 2/3 of body cells to take up glucose from the bloodstream through the GLUT4 transporter, thus decreasing blood sugar levels.
Diabetes mellitus describes a group of chronic metabolic diseases in which the person has a high blood glucose level, either because insulin production is inadequate or because the body's cells do not respond properly to insulin (also called insulin resistance) or both. Diabetes can be divided into two types: type 1 and type 2.
Type 1 diabetes:
The human body does not produce insulin. This type of diabetes is also called insulin-dependent diabetes, juvenile diabetes or early-onset diabetes. People usually develop type 1 diabetes before their 40th year, often in early adulthood or teenage years.
Patients with type 1 diabetes will need to take insulin injections for the rest of their life. They must also ensure proper blood-glucose levels by carrying out regular blood tests and following a special diet. Type 1 diabetes is not curable and is generally a form which is less common than type 2.
Type 2 diabetes:
In type 2 diabetes the body does not respond properly to insulin. Type 2 diabetes occurs mainly in the elderly and in people who are overweight (BMI>25). The treatment of type 2 diabetes is the first of dietary advice in conjunction with achieving a healthy weight (BMI = 18.5-25). Unlike type 1, type 2 is curable. Type 2 diabetes is also referred to as non-insulin-dependent diabetes mellitus.
Approximately 90% of all cases of diabetes worldwide are of this type.
These are the consequences that many diabetics may experience:
- Amputation of limbs
- Depression
- Heart diseases
- Skin problems
- Gastrointestinal problems
- Kidney disease
- Eye problems
- Problems of the joints
- Problems with brains
- Sexual problems
- Foot problems
- Nerves disorders
Dietary guidelines for diabetes prevention:
- Choose products with minimum 1.5 grams of fiber per 100 kcal, products with maximum 30 En% fat, products with maximum 7 En% saturated fat, products with 10-20 En% protein, products with maximum 10 En% sugars and products with a low GI value (55 or lower) or in other words, your daily diet (=all meals/products that you eat on a daily basis) should on average contain minimum 1.5 grams of fiber per 100 kcal, maximum 30 En% fat, maximum 7 En% saturated fat, 10-20 En% protein and maximum 10 En% sugars.
- Aim for a healthy weight. A healthy weight has a BMI of 18.5-25. BMI is weight divided by height squared (weight (kg)/height2 (m)).
- Spend at least 60-90 minutes of physical activities per day or at least 10000 steps per day.
- Eat at least 3 times (100-150 g fish per time) a week oily fish. Oily fishes are sardines, herring, salmon, anchovies, eel and mackerel. Oily fish contains more EPA and DHA than non-oily fish.
- Eat 300 grams of vegetables and five servings of fruit a day or 30-40 grams of fiber per day.
40 grams of fiber per dag corresponds to a daily diet of minimum 2 grams of fiber per 100 kcal. - Eat plenty of whole grains, such as brown bread and oatmeal and legumes.
- Limit to 2-3 glasses of alcohol for men and 1-2 glasses for women a day or <30 g alcohol per day.