Objectives:
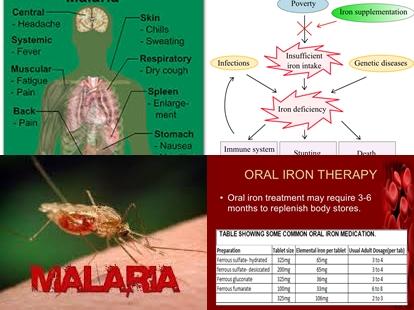
Iron-deficiency anaemia is common during childhood. Iron administration has been claimed to increase the risk of malaria. Therefore, this meta-analysis (review article) has been conducted.
Does iron administration with or without folic acid, increase malaria risk in children living in areas with hyperendemic or holoendemic malaria transmission?
Study design:
This review article included 35 RCTs comprising 31,955 children younger than 18 years of age.
Results and conclusions:
The investigators found in 14 trials with 7168 children that overall, iron administration did cause an excess of clinical malaria [risk ratio = 0.93, 95% CI = 0.87 to 1.00; high quality evidence].
The investigators found iron administration probably did not cause an excess of clinical malaria in both populations where anaemia is common and those in which anaemia is uncommon.
The investigators found in 7 trials with 5,586 participants conducted in areas where there are prevention and management services for malaria that iron administration (with or without folic acid) significantly reduced clinical malaria risk with 9% [RR = 0.91, 95% CI = 0.84 to 0.97; low quality evidence].
However, in areas where such services are unavailable, iron administration (with or without folic acid) significantly increased the incidence of malaria [RR = 1.16, 95% CI = 1.02 to 1.31; nine trials, 19,086 participants, low quality evidence].
The investigators found in 3 RCTs with 728 children that iron administration and antimalarial treatment significantly reduced clinical malaria risk with 46% [RR = 0.54, 95% CI = 0.43 to 0.67, I2 = 0%; high quality evidence].
However, there was no difference in the risk of death [RR = 1.05, 95% CI = 0.52 to 2.11].
The investigators found overall, iron administration resulted in fewer anaemic children at follow up and the end average change in haemoglobin from base-line was higher with iron administration.
The investigators concluded there was no increased risk of clinical malaria and parasitaemia, all-cause mortality, or other infectious complications with iron supplementation alone for children living in areas with intense malaria transmission. However, iron supplementation may be associated with an increased risk of malaria in settings with no access to malaria prevention or management services, but is safe when such services are available. In such circumstances, administration of iron with an antimalarial drug confers significant protection from malaria and probably reflects the effect of the antimalarial drugs. Furthermore, iron supplementation significantly improves haemoglobin levels and reduces the prevalence of anaemia in highly malaria-endemic areas. Universal screening for iron deficiency and anaemia can select the population most likely to benefit from iron administration, but such screening programmes are not currently feasible in most areas with intense malaria transmission.
Original title:
Oral iron supplements for children in malaria-endemic areas by Neuberger A, Okebe J, […], Paul M.
Link:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4916933/
Additional information of El Mondo:
Find more information/studies on food fortification/malnutrition and iron right here.