Purified anthocyanin supplements reduce cardiovascular risk

Objectives:
The associations between intake of anthocyanins and anthocyanin-rich berries and cardiovascular risks remained to be established. Therefore, this review article has been conducted.
Do purified anthocyanin supplements and dietary intakes of anthocyanin-rich berries reduce cardiovascular risk?
Study design:
This review article included 44 eligible RCTs consisting of 52 comparison groups and 2,353 subjects and 15 prospective cohort studies with 5,54,638 subjects (persons).
7 of the 44 RCTs were crossover trials with the rest parallel-designed.
15 of the included studies investigated the effects of purified anthocyanins, all of which were produced from berries. For the remaining anthocyanin-rich berry studies, interventions were blueberry in 13 studies, cranberry in 12 studies, bilberry in 3 studies and blackcurrant in 1 study.
The intervention durations ranged from 2 weeks to 24 months with a median of 8 weeks.
24 of the 44 RCTs were rated as high quality with the others as low to moderate quality.
The follow-up periods of 15 cohort studies ranged from 4.3 to 24 years with a median of 12 years. Most of the included cohort studies used FFQ to assess dietary anthocyanin intake and only 3 of them used dietary records.
12 of the 15 cohort studies were rated as high quality.
There was no publication bias, except for the effects of purified anthocyanins on HDL cholestrerol levels [Begg's p = 0.016].
Results and conclusions:
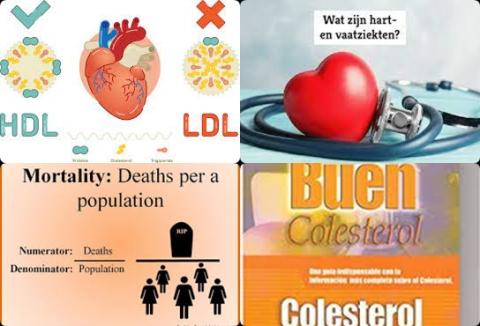
The investigators found pooled analysis of RCTs showed that purified anthocyanin supplements significantly reduced blood LDL cholesterol (bad cholesterol) concentrations [WMD = -5.43 mg/dL, 95% CI = -8.96 to -1.90 mg/dL, p = 0.003].
The investigators found pooled analysis of RCTs showed that purified anthocyanin supplements significantly reduced triglyceride concentrations [WMD = -6.18 mg/dL, 95% CI = -11.67 to -0.69 mg/dL, p = 0.027, I2 = 0%].
The investigators found pooled analysis of RCTs showed that purified anthocyanin supplements significantly increased HDL cholesterol (good cholesterol) concentrations [WMD = 2.76 mg/dL, 95% CI = 1.34 to 4.18 mg/dL, p 0.001, I2 = 43.5%].
Subgroup analysis showed that the effects on HDL cholesterol concentrations were not significantly influenced by study duration, health status of subjects, anthocyanin doses, study quality and funding source.
The investigators found pooled analysis of RCTs showed that purified anthocyanin supplements significantly reduced tumor necrosis factor alpha concentrations [WMD = -1.62 pg/mL, 95% CI = -2.76 to -0.48 pg/mL, p = 0.005, I2 = 0%].
The investigators found pooled analysis of RCTs showed that purified anthocyanin supplements significantly reduced C-reactive protein concentrations [WMD = -0.028 mg/dL, 95% CI = -0.050 to -0.005 mg/dL, p = 0.014, I2 = 26%].
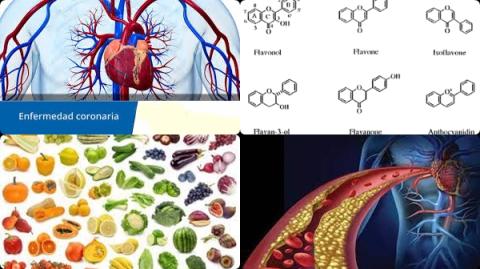
The investigators found pooled analysis of RCTs showed administration of anthocyanin-rich berries (blueberry, cranberry, bilberry and blackcurrant) significantly reduced blood total cholesterol concentrations [WMD = -4.48 mg/dL, 95% CI = -8.94 to -0.02 mg/dL, p = 0.049].
The investigators found pooled analysis of RCTs showed administration of anthocyanin-rich berries (blueberry, cranberry, bilberry and blackcurrant) significantly reduced C-reactive protein concentrations [WMD = -0.046 mg/dL, 95% CI = -0.070 to -0.022 mg/dL, p 0.001, I2 = 0%].
The investigators found pooled analysis of cohort studies showed high dietary anthocyanins intakes significantly reduced risk of coronary heart disease (CHD) with 17% [relative risk = 0.83, 95% CI = 0.72 to 0.95, p = 0.009, I2 = 51.2%].
The investigators found pooled analysis of cohort studies showed high dietary anthocyanins intakes significantly reduced risk of total cardiovascular disease incidence with 27% [relative risk = 0.73, 95% CI = 0.55 to 0.97, p = 0.03, I2 = 76.7%].
The investigators found pooled analysis of cohort studies showed high dietary anthocyanins intakes significantly reduced risk of cardiovascular disease deaths with 9% [relative risk = 0.91, 95% CI = 0.87 to 0.96, p 0.001, I2 = 0%].
Subgroup analysis revealed that the protective roles of dietary anthocyanins against cardiovascular disease deaths was only found in women [RR = 0.89, 95% CI = 0.82 to 0.96, p = 0.003, I2 = 0.0%] and not in men [RR = 0.92, 95% CI = 0.79 tot 1.07, p = 0.263, I2 = 0.0%].
The investigators concluded current clinical and epidemiological evidence show the protective roles of purified anthocyanin supplements during 8 weeks and anthocyanin-rich berries (blueberry, cranberry, bilberry and blackcurrant) on cardiovascular health. These results suggest that regular consumption of either purified anthocyanins or anthocyanin-rich berries could prevent cardiovascular disease through their lipid-lowering and anti-inflammatory properties. Therefore, anthocyanins and anthocyanin-rich berries should be taken into consideration when formulating cardioprotective diets in the future.
Original title:
Anthocyanins, Anthocyanin-Rich Berries, and Cardiovascular Risks: Systematic Review and Meta-Analysis of 44 Randomized Controlled Trials and 15 Prospective Cohort Studies by Xu L, Tian Z, […], Yang Y.
Link:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8714924/
Additional information of El Mondo:
Find more information/studies on anthocyanins, lowering cholesterol levels and cardiovascular disease right here.