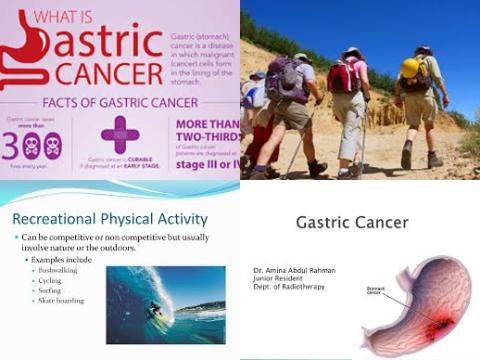
Recreational physical activity reduces risk of gastric cancer
Objectives:
Does physical activity reduce gastric cancer risk?
Study design:
This review article included 7 cohort studies (with mean reported follow-up ranging from 6 to 18.8 years) and 9 case control studies reporting 11,111 cases of gastric cancer among 1,606,760 patients.
There was no evidence of publication bias, both quantitatively [Begg and Mazumdar rank correlation test, p = 0.62] and qualitatively, on visual inspection of the funnel plot.
Results and conclusions:
The investigators found the risk of gastric cancer was 21% [OR = 0.79, 95% CI = 0.71-0.87, I2 = 55%] lower among the most physically active people as compared with the least physically active people, after adjustment for important confounders, including age, obesity, and other risk factors for gastric cancer (smoking, alcohol, dietary patterns and socioeconomic status).
This protective effect was seen for gastric cancers in the cardia [OR = 0.80, 95% CI = 0.63-1.00, 4 studies] and distal stomach [OR = 0.63, 95% CI = 0.52-0.76, 5 studies].
The investigators found increasing physical activity was associated with a reduced risk of gastric cancer in both men [OR = 0.86, 95% CI = 0.75-0.99, 10 studies] and women [OR = 0.72, 95% CI = 0.55-0.94, 3 studies].
The investigators found in 12 studies that increased recreational physical activity showed an 18% reduction in gastric cancer risk [OR = 0.82, 95% CI = 0.72-0.94].
The investigators found the effect size was significantly smaller in high-quality studies [OR = 0.86, 95% CI = 0.75-0.99, 6 studies] as compared with low-quality studies [OR = 0.74, 95% CI = 0.69-0.81, 10 studies]. The results were consistent across sex, study quality, study design and geographic location.
The investigators concluded physical activity - especially recreational physical activity - is associated with reduced risk of gastric cancer. Lifestyle interventions focusing on increasing physical activity may decrease the global burden of gastric cancer, in addition to a myriad of other health benefits with being physically active, which include cardiovascular, metabolic and psychologic wellbeing.
Original title:
Physical Activity Is Associated with Reduced Risk of Gastric Cancer: A Systematic Review and Meta-analysis by Singh S, Varayil JE, […], Iyer PG.
Link:
http://cancerprevention.aacrjournals.org/content/7/1/12.abstract
Additional information of El Mondo:
Find more studies/information on physical activity and cancer right here.