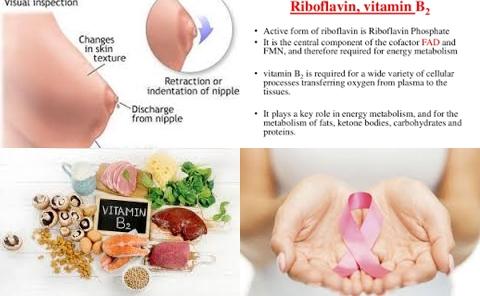
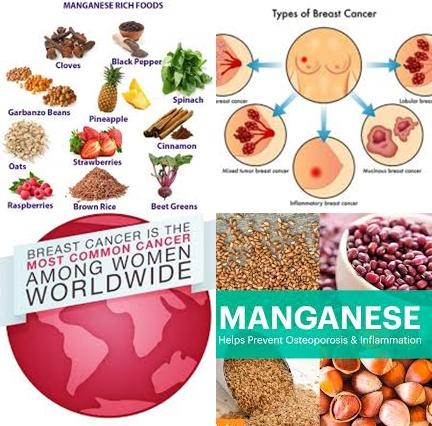
Manganese deficiency may increase breast cancer
Objectives:
There are conflicting reports on the correlation between manganese (Mn) levels and breast cancer. Therefore, this review article (meta-analysis) has been conducted.
Does manganese deficiency increase risk of breast cancer?
Study design:
This review article included 11 case-control studies involving 1302 subjects.
There was no evidence of publication bias. Sensitivity analysis showed that excluding any one study from the pooled analysis did not vary the results substantially.
Results and conclusions:
The investigators found the random-effects meta-analysis results indicated that subjects with breast cancer had lower manganese levels in serum and hair than healthy controls [SMD = -1.51, 95% CI = -2.47 to -0.56, I2 = 97.8%, p 0.001].
The investigators found in subgroup analysis that subjects with breast cancer had lower manganese levels than healthy controls in China [SMD = -1.32, 95% CI = -2.33 to -0.32] and Korea [SMD = -4.08, 95% CI = -4.63 to -3.54], but not in Turkey [SMD = -0.96, 95% CI = -3.19 to 1.27].
The investigators found in subgroup analysis that the differences of manganese levels between patients with breast cancer and healthy controls were similar in different sample specimens:
serum [SMD = -1.24, 95% CI = -2.31 to -0.16];
hair [SMD = -1.99, 95% CI = -3.91 to -0.06] and;
different types of manganese measurement:
ICP-AAS [SMD = -1.14, 95% CI = -2.24 to -0.04];
GFAAS [SMD = -1.94, 95% CI = -2.38 to -1.49];
ICP-AES [SMD = -3.77, 95% CI = -4.70 to -2.85]. These findings can well explain that the between-study variability was the main source of heterogeneity.
The investigators concluded there is an association between deficient manganese concentration and breast cancer. However, the subgroup analysis found that there was contradiction regarding races and geography, like China and Turkey. Thus this finding needs further confirmation by trans-regional multicenter, long-term observation in a cohort design to obtain better understanding of causal relationships between manganese levels and breast cancer, through measuring manganese at baseline to investigate whether the highest manganese category versus lowest was associated with breast cancer risk.
Original title:
The association between deficient manganese levels and breast cancer: a meta-analysis by Shen F, Cai WS, [...],Xu B.
Link:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4443096/
Additional information of El Mondo:
Find more studies/information on manganese and breast cancer right here.