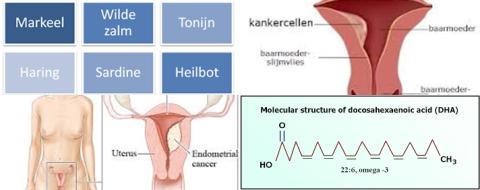
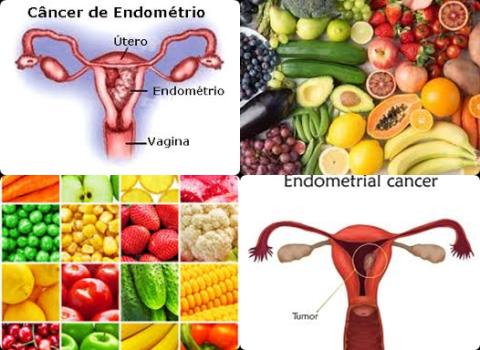
Fruits and vegetables reduce endometrial cancer
Objectives:
Does consumption of fruits and vegetables reduce risk of endometrial cancer?
Study design:
This review article included of 21 case-control studies and 6 cohort studies.
Results and conclusions:
The investigators found that vegetables consumption significantly reduced risk of endometrial cancer with 24% [pooled odds ratio [OR], relative risk [RR], hazard ratio [HR] = 0.76, 95% CI = 0.63 to 0.91].
The investigators found that cruciferous vegetables consumption significantly reduced risk of endometrial cancer with 19% [pooled OR = 0.81, 95% CI = 0.70 to 0.94].
The investigators found that dark green and yellow/orange combined vegetables consumption significantly reduced risk of endometrial cancer with 36% [pooled OR = 0.64, 95% CI = 0.42 to 0.97].
The investigators found that fruits consumption significantly reduced risk of endometrial cancer with 19% [pooled OR = 0.81, 95% CI = 0.70 to 0.92].
The investigators found these results were primarily based on studies of high quality and exhibited either by case-control only or a combination of case-control and cohort studies. Additionally, the results varied by geographic location, such as Western areas, the US and Italy.
The investigators concluded that consumption of fruits and vegetables has beneficial effects on endometrial cancer risk and that specific kinds of fruits and vegetables should be recommended differently due to their outstanding bioactive components.
Original title:
The influence of dietary vegetables and fruits on endometrial cancer risk: a meta-analysis of observational studies by Lu YT, Gunathilake M and Kim J.
Link:
https://pubmed.ncbi.nlm.nih.gov/36151331/
Additional information of El Mondo:
Find more information/studies on cancer and fruit and vegetable consumption right here.