Objectives:
Intervention studies suggest that incorporating walnuts into the diet may improve blood lipids without promoting weight gain. Therefore, this review article has been conducted.
Does a diet with walnuts improve blood lipids profile (such as cholesterol and triglycerides) without promoting weight gain?
Study design:
This review article included 26 clinical trials with a total of 1,059 participants.
Weighted mean differences (WMDs) were used.
Results and conclusions:
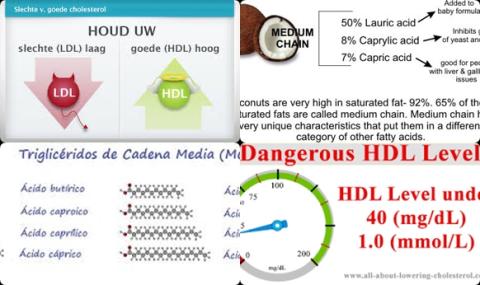
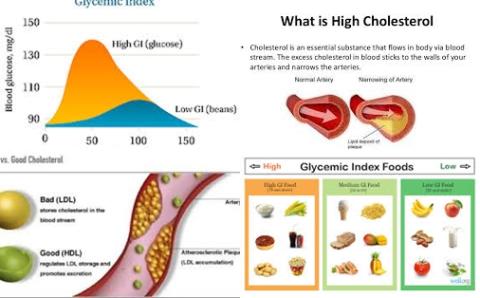
The investigators found compared with control group, a walnut-enriched diet significantly reduced total blood cholestrerol level with 6.99 mg/dL [95% CI = -9.39 to -4.58 mg/dL, p 0.001; 3.25% greater reduction].
The investigators found compared with control group, a walnut-enriched diet significantly reduced low-density lipoprotein (LDL) cholesterol level with 5.51 mg/dL [95% CI = -7.72 to -3.29 mg/dL, p 0.001; 3.73% greater reduction].
The investigators found compared with control group, a walnut-enriched diet significantly reduced triglyceride concentrations with 4.69 mg/dL [WMD = -4.69 mg/dL, 95% CI = -8.93 to -0.45 mg/dL, p = 0.03; 5.52% greater reduction].
The investigators found more pronounced reductions in blood lipids were observed when walnut interventions were compared with American and Western diets [WMD for total blood cholestrerol level = -12.30, 95% CI = -23.17 to -1.43] and for LDL blood cholestrerol level = -8.28, 95% CI = -13.04 to -3.51, p 0.001].
The investigators found apolipoprotein B was also reduced significantly more on walnut-enriched diet compared with control group [WMD = -3.74 mg/dL, 95% CI = -6.51 to -0.97 mg/dL, p = 0.008].
The investigators found a trend towards a reduction was observed for apolipoprotein A [WMD = -2.91, 95% CI = -5.98 to 0.08, p = 0.057].
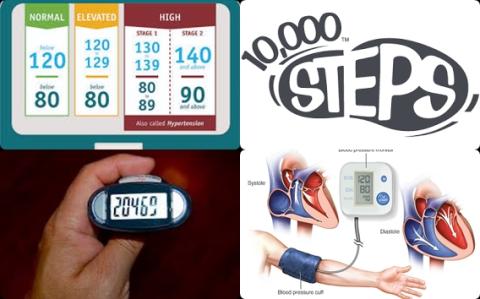
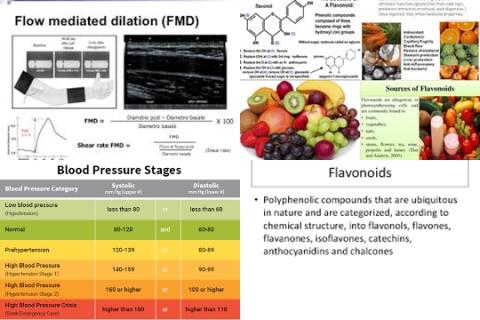
The investigators found, however, walnut-enriched diet did not lead to significant differences in weight change compared with control diet [WMD = -0.12 kg, 95% CI = -2.12 to 1.88, p = 0.90], systolic blood pressure [WMD = -0.72 mmHg, 95% CI = -2.75 to 1.30, p = 0.48] or diastolic blood pressure [WMD = -0.10 mmHg, 95% CI = -1.49 to 1.30, p = 0.88].
The investigators concluded that walnut-enriched diet improves total and LDL cholesterol levels (bad cholesterol), apolipoprotein B levels and triglyceride levels without adversely affecting body weight or blood pressure.
Original title:
Effects of walnut consumption on blood lipids and other cardiovascular risk factors: an updated meta-analysis and systematic review of controlled trials by Guasch-Ferré M, Li J, […], Tobias DK.
Link:
https://www.ncbi.nlm.nih.gov/pubmed/29931130
Additional information of El Mondo:
Find more information/studies on review article/significantly, nut consumption and cholesterol right here.
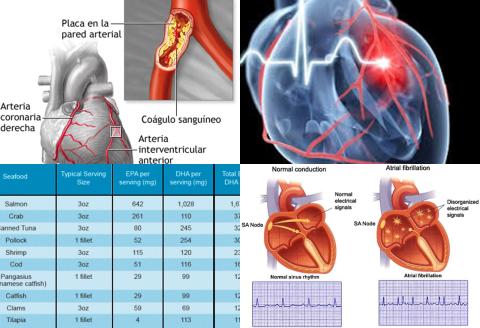
Persons with atherosclerosis often have an elevated total cholesterol level, an elevated LDL cholesterol level, an elevated triglyceride level and an elevated apolipoprotein B level.
Persons with atherosclerosis are advised to choose products/meals with maximum 30 En% fat, maximum 7 En% saturated fat, maximum 0.2 gram salt per 100 kcal and minimum 1.5 grams fiber per 100 kcal. Check here which products/meals are suitable for persons with atherosclerosis.