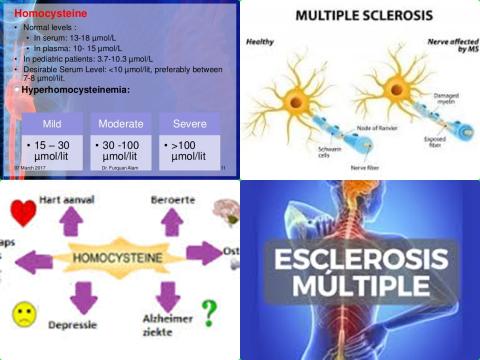
Higher serum levels of homocysteine increase multiple sclerosis
Objectives:
Multiple sclerosis (MS) is a demyelinating and disabling inflammatory disease of the central nervous system. Multiple sclerosis is triggered by complex environmental factors which mostly affect genetically the susceptible young people. Emerging data has suggested that changes of homocysteine (Hcy), vitamin B12 and folate serum levels may be associated with multiple sclerosis. However, previous findings are not always consistent. Therefore, this review aricle has been conducted.
Does a low serum homocysteine, vitamin B12 or folate level increase risk of multiple sclerosis?
Study design:
This review article included 21 original studies with 1,738 multiple sclerosis patients and 1,424 controls (patients without multiple sclerosis). There were 17 studies for measuring homocysteine, 16 studies for measuring vitamin B12 and 13 studies for measuring folate in patients with multiple sclerosis, respectively.
Results and conclusions:
The investigators found patients with multiple sclerosis (MS) had higher serum levels of homocysteine [SMD = 0.64, 95% CI = 0.33 to 0.95, p 0.0001] compared with control groups.
The investigators found no significant differences of SMD for vitamin B12 [SMD = -0.08, 95% CI = -0.35 to 0.20, p = 0.58] or folate [SMD = 0.07, 95% CI = -0.14 to 0.28, p = 0.52] between MS and controls.
The investigators found subgroup analysis demonstrated that there was statistically significant difference for homocysteine between relapsing-remitting MS (RRMS) patients and controls with a SMD of 0.67 [95% CI = 0.21 to 1.13, p = 0.004].
However, no significant difference of homocysteine serum levels between secondary progressive MS patients or primary progressive MS patients and controls.
The investigators found no significant difference of homocysteine levels in females [SMD = 0.22, 95% CI = -0.16 to 0.60, p = 0.25] or males [SMD = 0.56, 95% CI = -0.13 to 1.26, p = 0.11] between MS patients and controls.
The investigators concluded higher serum levels of homocysteine increase risk of multiple sclerosis (MS), especially for relapsing-remitting MS (RRMS) patients. Functional studies are required to assess the effects of homocysteine on patients with MS at the molecular level.
Original title:
Serum levels of Homocysteine, Vitamin B12 and Folate in Patients with Multiple Sclerosis: an Updated Meta-Analysis by Li X, Yuan J, [...], Hu W.
Link:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7085269/
Additional information of El Mondo:
Find here more information/studies about lowering serum levels of homocysteine.