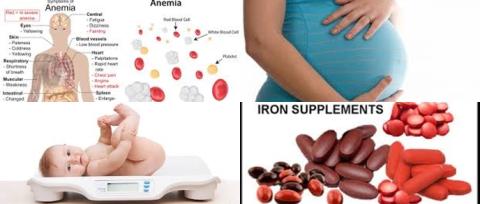
Daily 10 to 66 mg iron supplementation during pregnancy improve maternal haematological status and birth weight
Objectives:
Does iron supplementation during pregnancy improve maternal haematological status and birth weight?
Study design:
This review article included 48 RCTs (17,793 women) and 44 cohort studies (1,851,682 women).
The dose of iron in RCTs ranged from 10 mg to 240 mg daily. Duration of supplementation varied from 7 to 8 weeks up to 30 weeks during pregnancy.
Significant heterogeneity existed for several outcomes that could not be explained substantially by pre-specified subgroups.
Results and conclusions:
The investigators found iron supplementation during pregnancy increased maternal mean haemoglobin concentration by 4.59 g/L [95% CI = 3.72 to 5.46] compared with controls.
The investigators found iron with folic acid was associated with a significant increase in mean haemoglobin concentration of 10.41 g/L [95% CI = 5.36 to 15.46, I2 = 0%, 9 trials] and reduction in risk of anaemia in the third trimester or at delivery of 56% [95% CI = 0.37 to 0.53, I2 = 44%, 5 trials]. Significant means there is an association with a 95% confidence.
The investigators found iron supplementation during pregnancy significantly reduced the risk of anaemia with 50% [95% CI = 0.42 to 0.59] compared with controls.
The investigators found iron supplementation during pregnancy significantly reduced the risk of iron deficiency (of the mother) with 41% [95% CI = 0.46 to 0.79] compared with controls.
The investigators found iron supplementation during pregnancy significantly reduced the risk of iron deficiency anaemia with 60% [95% CI = 0.26 to 0.60] compared with controls.
The investigators found iron supplementation during pregnancy significantly reduced the risk of low birth weight (2500 g) with 19% [95% CI = 0.71 to 0.93] compared with controls.
However, the investigators found iron supplementation during pregnancy non-significantly reduced the risk of preterm birth with 16% [95% CI = 0.68 to 1.03] compared with controls. Non-significant means there is no association with a 95% confidence.
The investigators found in cohort studies that anaemia in the first or second trimester was significantly associated with a higher risk for low birth weight of 29% [adjusted odds ratio 1.29, 95% CI = 1.09 to 1.53] and preterm birth with 21% [adjusted odds ratio = 1.21, 95% CI = 1.13 to 1.30].
The investigators found in exposure-response analysis that for every 10 mg increase in iron dose/day, up to 66 mg/day, the relative risk of maternal anaemia was significantly 0.88 [95% CI = 0.84 to 0.92, p for linear trend 0.001].
The investigators found in exposure-response analysis that birth weight increased by 15.1 g [95% CI = 6.0 to 24.2, p for linear trend = 0.005] and risk of low birth weight significantly decreased by 3% [relative risk = 0.97, 95% CI = 0.95 to 0.98, p for linear trend 0.001] every 10 mg increase in dose/day.
Furthermore, the investigators found for each 1 g/L increase in mean haemoglobin, birth weight increased by 14.0 g [95% CI = 6.8 to 21.8, p for linear trend = 0.002]. However, mean haemoglobin was not associated with the risk of low birth weight and preterm birth.
The investigators found no evidence of a significant effect on duration of gestation, small for gestational age births and birth length and duration of iron use was not significantly associated with the outcomes after adjustment for dose.
The investigators concluded daily prenatal use of iron substantially improved birth weight in a linear dose-response fashion, probably leading to a reduction in risk of low birth weight. An improvement in prenatal mean haemoglobin concentration linearly increased birth weight and a linear decrease in maternal anaemia with higher doses of iron, up to 66 mg/day.
Original title:
Anaemia, prenatal iron use, and risk of adverse pregnancy outcomes: systematic review and meta-analysis by Haider BA, Olofin I, […], Fawzi WW.
Link:
http://www.bmj.com/content/346/bmj.f3443
Additional information of El Mondo:
Find more information/studies on iron and pregnancy right here.
Iron deficiency anaemia occurs when there isn't enough iron in the body. Anaemia is a condition where the amount of haemoglobin in the blood is below the normal level.
Iron deficiency anaemia has been defined as haemoglobin 110 g/L and serum ferritin 12 µg/L.