Objectives:
The associations of various dietary or circulating antioxidants with the risk of all-cause mortality in the general population have not been established yet. Therefore, this review article has been conducted.
Do dietary or circulating antioxidants reduced risk of all-cause mortality in the general population?
Study design:
This review article included 41 prospective observational studies with a total of 507,251 participants and 73,965 cases of all-cause mortality.
Results and conclusions:
The investigators found for the highest compared with the lowest category of circulating total carotenes concentrations a significantly reduced risk of 40% [RR = 0.60, 95% CI = 0.46 to 0.74] for all-cause mortality.
The investigators found for the highest compared with the lowest category of circulating vitamin C concentrations a significantly reduced risk of 39% [RR = 0.61, 95% CI = 0.53 to 0.69] for all-cause mortality.
The investigators found for the highest compared with the lowest category of circulating selenium concentrations a significantly reduced risk of 38% [RR = 0.62, 95% CI = 0.45 to 0.79] for all-cause mortality.
The investigators found for the highest compared with the lowest category of circulating β-carotene concentrations a significantly reduced risk of 37% [RR = 0.63, 95% CI = 0.57 to 0.70] for all-cause mortality.
The investigators found for the highest compared with the lowest category of circulating α-carotene concentrations a significantly reduced risk of 32% [RR = 0.68, 95% CI = 0.58 to 0.78] for all-cause mortality.
The investigators found for the highest compared with the lowest category of circulating total carotenoids concentrations a significantly reduced risk of 32% [RR = 0.68, 95% CI = 0.56 to 0.80] for all-cause mortality.
The investigators found for the highest compared with the lowest category of circulating lycopene concentrations a significantly reduced risk of 25% [RR = 0.75, 95% CI = 0.54 to 0.97] for all-cause mortality.
The investigators found for the highest compared with the lowest category of circulating α-tocopherol concentrations a significantly reduced risk of 16% [RR = 0.84, 95% CI = 0.77 to 0.91] for all-cause mortality.
The investigators found for the highest compared with the lowest category of dietary intakes of total carotenoids a significantly reduced risk of 24% [RR = 0.76, 95% CI = 0.66 to 0.85] for all-cause mortality.
The investigators found for the highest compared with the lowest category of dietary intakes of total antioxidants a significantly reduced risk of 23% [RR = 0.77, 95% CI = 0.73 to 0.81] for all-cause mortality.
The investigators found for the highest compared with the lowest category of dietary intakes of selenium a significantly reduced risk of 21% [RR = 0.79, 95% CI = 0.73 to 0.85] for all-cause mortality.
The investigators found for the highest compared with the lowest category of dietary intakes of α-carotene a significantly reduced risk of 21% [RR = 0.79, 95% CI = 0.63 to 0.94] for all-cause mortality.
The investigators found for the highest compared with the lowest category of dietary intakes of β-carotene a significantly reduced risk of 18% [RR = 0.82, 95% CI = 0.77 to 0.86] for all-cause mortality.
The investigators found for the highest compared with the lowest category of dietary intakes of vitamin C a significantly reduced risk of 12% [RR = 0.88, 95% CI = 0.83 to 0.94] for all-cause mortality.
The investigators found for the highest compared with the lowest category of dietary intakes of total carotenes a significantly reduced risk of 11% [RR = 0.89, 95% CI = 0.81 to 0.97] for all-cause mortality.
The investigators found for the highest compared with the lowest category a nonsignificant inverse association between dietary zinc, zeaxanthin, lutein and vitamin E and all-cause mortality risk.
The investigators found in nonlinear dose-response meta-analyses a linear inverse association in the analyses of dietary β-carotene and total antioxidant capacity, as well as in the analyses of circulating α-carotene, β-carotene, selenium, vitamin C and total carotenoids.
The investigators found the association appeared to be U-shaped in the analyses of serum lycopene and dietary vitamin C.
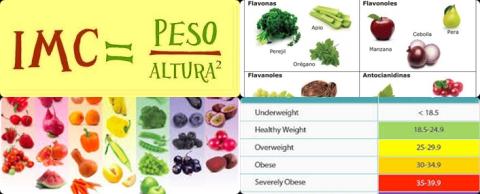
The investigators concluded that a diet with high antioxidant properties reduces the risk of all-cause mortality. These findings confirm current recommendations that promote higher intake of antioxidant-rich foods such as fruit and vegetables.
Original title:
Dietary Antioxidants, Circulating Antioxidant Concentrations, Total Antioxidant Capacity, and Risk of All-Cause Mortality: A Systematic Review and Dose-Response Meta-Analysis of Prospective Observational Studies by Jayedi A, Rashidy-Pour A, […], Shab-Bidar S.
Link:
https://www.ncbi.nlm.nih.gov/pubmed/30239557
Additional information of El Mondo:
Find more information/studies on meta-analysis/cohort studies, nutrients, antioxidants and elderly right here.