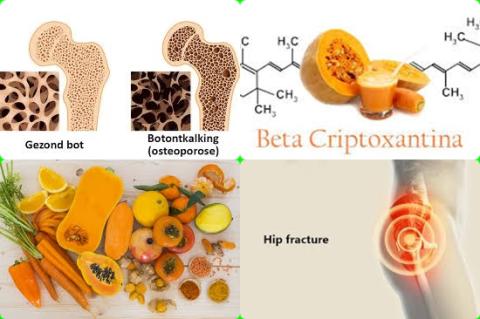
100 µg/d vitamin K2 + 1000 mg/d calcium supplements increase lumbar spine bone mineral

Objectives:
With the increasing incidence of osteoporosis, vitamin K and calcium have been linked to bone mineral density (BMD) and undercarboxylated osteocalcin (UcOC) in many studies, but the results of studies of the combined effect of vitamin K and calcium on BMD and UcOC in humans have been inconsistent. Therefore, this review article has been conducted.
Do vitamin K and calcium supplements used in combination increase bone mineral density and decrease undercarboxylated osteocalcin level?
Study design:
This review article included 10 randomized controlled trials (RCTs) with a total of 1,346 patients.
Results and conclusions:
The investigators found that the combination of vitamin K and calcium supplements was significantly associated with a higher lumbar spine bone mineral density [SMD = 0.20, 95% CI = 0.07 to 0.32, I2 = 46.9%, p = 0.049].
However, after applying trim and fill method (where correction was made for publication bias), the results were not statistically significant [estimate = 0.067, 95% CI = -0.044 to 0.178].
The investigators found that vitamin K and calcium supplementation led to a significant decrease in undercarboxylated osteocalcin [SMD = -1.71, 95% CI = - 2.45 to -0.96, I2 = 95.7%, p 0.01].
The results did not change after correcting publication bias [estimate = - 0.947, 95% CI = -1.211 to - 0.687].
The SMD in the sensitivity analysis was -0.82 [95% CI = - 1.10 to -0.55, I2 = 65.4%, p 0.01].
The investigators found in subgroup analysis that the combination of vitamin K2 and calcium supplements was significantly associated with a higher lumbar spine bone mineral density [SMD = 0.30, 95% CI = 0.10 to 0.51, I2 = 0%].
The investigators found in subgroup analysis that the combination of vitamin K and ≤ 1000 mg/d calcium supplements was significantly associated with a higher lumbar spine bone mineral density [SMD = 0.19, 95% CI = 0.05 to 0.32, I2 = 62.3%].
The investigators found in subgroup analysis that the combination of ≤100 µg/d vitamin K and calcium supplements was significantly associated with a higher lumbar spine bone mineral density [SMD = 0.40, 95% CI = 0.20 to 0.61, I2 = 49.9%].
The investigators found in subgroup analysis that the combination of vitamin K and calcium supplements during ≤1 year was significantly associated with a higher lumbar spine bone mineral density [SMD = 0.38, 95% CI = 0.19 to 0.57, I2 = 40%].
The investigators concluded that ≤100 µg/d vitamin K2 and ≤1000 mg/d calcium supplements used in combination are associated with a higher lumbar spine bone mineral density and a lower undercarboxylated osteocalcin level.
Original title:
The combined effect of vitamin K and calcium on bone mineral density in humans: a meta-analysis of randomized controlled trials by Hu L, Ji J, [...], Yu B.
Link:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8515712/
Additional information of El Mondo:
Find more information/studies on review article/RCTs/publication bias, vitamin K, calcium and increasing bone mineral density right here.