High dietary intake of vitamin E reduces dementia
Objectives:
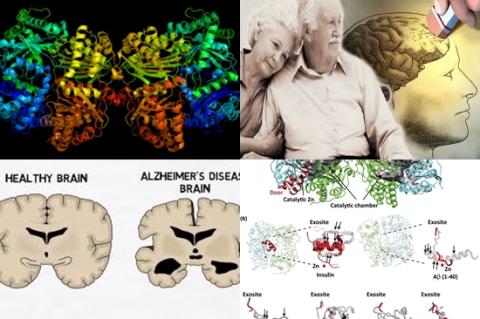
Dementia is a chronic progressive neurodegenerative disease that can lead to disability and death in humans, but there is still no effective prevention and treatment. Due to the neuroprotective effects of vitamin E, a large number of researchers have explored whether vitamin E can reduce the risk of dementia. Some researchers believe that vitamin E can reduce the risk of dementia, while others hold the opposite conclusion. Therefore, this review article has been conducted.
Do high intakes of diet or vitamin E supplements reduce the risk of dementia?
Study design:
This review article included 13 cohort studies (46,968 participants and 6,046 dementia patients after 4-23 years of follow-up) and 2 case-control studies with (3,157 controls and 3,459 patients).
The studies included in this meta-analysis (review article) were published between 1983 and 2022.
The literary NOS quality score ranged from 6 to 8.
There was no publication bias.
Results and conclusions:
The investigators found a high intake of diet or vitamin E supplements significantly decreased the risk of dementia by 21% [OR = 0.79, 95% CI = 0.70 to 0.88, I2 = 35.0%, p = 0.071].
This decreased risk was also significant in cohort studies [OR = 0.79, 95% CI = 0.69 to 0.89], dietary intake of vitamin E [OR = 0.78, 95% CI = 0.65 to 0.95], vitamin E supplement [OR = 0.83, 95% CI = 0.73 to 0.94] and studies with NOS scores >7 [OR = 0.85, 95% CI = 0.75 to 0.97].
The investigators found a high intake of diet or vitamin E supplements significantly decreased the risk of Alzheimer's disease by 22% [OR = 0.78, 95% CI = 0.64 to 0.94, I2 = 36.9%, p = 0.123].
This decreased risk was also significant in cohort studies [OR = 0.77, 95% CI = 0.63 to 0.94].
The investigators found in sensitivity analysis the pooled ORs fluctuated within a certain range after deleting each study, indicating that the results of this meta-analysis were stable.
The investigators concluded high intakes of diet or vitamin E supplements reduce the risk of dementia. Therefore, the elderly can reduce the risk of dementia by appropriately increasing foods rich in vitamin E, but also pay attention to the toxic side effects of vitamin E. Although the results are reliable, they should be further validated by large RCTs.
Original title:
Association of vitamin E intake in diet and supplements with risk of dementia: A meta-analysis by Zhao R, Han X, [...], You H.
Link:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9376618/
Additional information of El Mondo:
Find more information/studies on dementia and vitamin E right here.