Daily 3 mg L-carnitine during 12 weeks reduce serum leptin concentrations in diabetic patients

Objectives:
The actual effects of L-carnitine administration on leptin serum level is inconsistent. Therefore, this review article (meta-analysis) has been conducted.
Does L-carnitine supplementation reduce leptin serum level?
Study design:
This review article included 7 RCTs with 325 cases (group with L-carnitine administration) and 330 controls (group without L-carnitine administration).
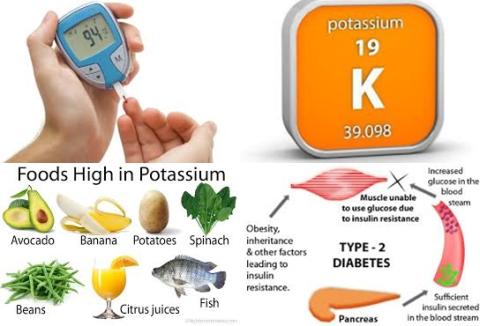
Subgroup analysis to find the sources of heterogeneity showed that L-carnitine dosage [ 2 g: I2 = 00.0%, p = 0.408] and study population [diabetes: I2 = 46.7%, p = 0.153 and non-diabetes: I2 = 15.1%, p = 0.317] were the potential sources of heterogeneity.
Results and conclusions:
The investigators found that L-carnitine supplementation had no significant effect on serum leptin concentrations [WMD = -0.565 ng/mL, 95% CI = -2.417 to 1.287, p = 0.550, I2 = 84.3%, p 0.0001].
The investigators found in subgroup analysis that ≥ 2 mg L-carnitine supplementation significantly reduced serum leptin concentrations [WMD = -2.742 ng/mL, 95% CI = -3.039 to -2.444, p 0.001].
The investigators found in subgroup analysis that L-carnitine supplementation significantly reduced serum leptin concentrations in diabetic patients [WMD = -2.946 ng/mL, 95% CI = -3.254 to -2.638, p 0.001].
The investigators found in subgroup analysis that L-carnitine supplementation during 12 weeks significantly reduced serum leptin concentrations [WMD = -2.772 ng/mL, 95% CI = -3.073 to -2.471, p 0.001].
The investigators concluded that at least 3 mg L-carnitine per day in the course of 12 weeks reduce serum leptin concentrations, especially in diabetic patients.
Original title:
The effect of L-carnitine supplementation on serum leptin concentrations: a systematic review and meta-analysis of randomized controlled trials by Nazary-Vannani A, Ghaedi E, […], Varkaneh HK.
Link:
https://www.ncbi.nlm.nih.gov/pubmed/29453657
Additional information of El Mondo:
Find more information/studies on diabetes and L-carnitine and diabetes right here.
L-carnitine is a non-essential amino acid, which is also found in foods.
|
Food |
Carnitine per 100g |
|---|---|
|
Beef steak, cooked, 4 ounces |
56-162 mg |
|
Ground beef, cooked, 4 ounces |
87-99 mg |
|
Milk, whole, 1 cup |
8 mg |
|
Codfish, cooked, 4 ounces |
4-7 mg |
|
Chicken breast, cooked, 4 ounces |
3-5 mg |
|
Ice cream, ½ cup |
3 mg |
|
Cheese, cheddar, 2 ounces |
2 mg |
|
Whole-wheat bread, 2 slices |
0.2 mg |
|
Asparagus, cooked, ½ cup |
0.1 mg |