Objectives:
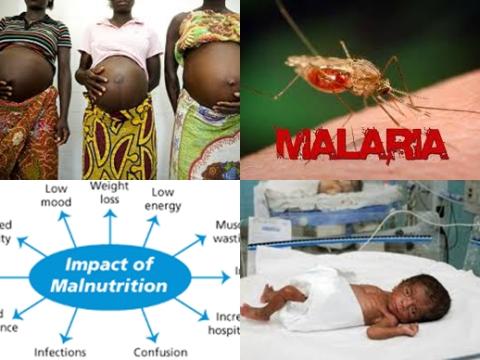
Four studies previously indicated that the effect of malaria infection during pregnancy on the risk of low birthweight (LBW 2,500g) may depend upon maternal nutritional status. Therefore, this review article has been conducted.
Does malaria during pregnancy increase risk of having a low birthweight and is there a synergistic interaction between malaria and malnutrition?
Study design:
This review article included pooled data from 14,633 pregnancies from 13 studies (6 cohort studies and 7 randomized controlled trials) conducted in Africa and the Western Pacific from 1996-2015.
The major limitations of the study included availability of only 2 cross-sectional measurements of malaria and the limited availability of ultrasound-based pregnancy dating to assess impacts on preterm birth and fetal growth in all studies.
Results and conclusions:
The investigators found the adjusted risk of delivering a baby with a low birthweight was 8.8% among women with malaria infection at antenatal enrollment compared to 7.7% among uninfected women [adjusted risk ratio = 1.14, 95% CI = 0.91 to 1.42, n = 13,613 pregnancies].
The investigators found the adjusted risk of delivering a baby with a low birthweight was 10.5% among women with malaria infection at delivery compared to 7.9% among uninfected women [adjusted risk ratio = 1.32, 95% CI = 1.08 to 1.62, n = 11,826 pregnancies].
The investigators found the adjusted risk of delivering a baby with a low birthweight was 15.3% among women with low mid-upper arm circumference (MUAC 23 cm) at enrollment compared to 9.5% among women with MUAC ≥ 23 cm [adjusted risk ratio = 1.60, 95% CI = 1.36 to 1.87, n = 9,008 pregnancies).
The investigators found the adjusted risk of delivering a baby with a low birthweight was 17.8% among women with both malaria infection and low mid-upper arm circumference at enrollment compared to 8.4% among uninfected women with mid-upper arm circumference ≥ 23 cm [joint adjusted risk ratio = 2.13, 95% CI = 1.21 to 3.73, n = 8,152 pregnancies].
The investigators found no evidence of synergism (i.e., excess risk due to interaction) between malaria infection and mid-upper arm circumference on the multiplicative [p = 0.5] or additive scale [p = 0.9]. Results were similar using body mass index (BMI) as an anthropometric indicator of nutritional status.
The investigators found meta-regression results indicated that there may be multiplicative interaction between malaria infection at enrollment and low mid-upper arm circumference within studies conducted in Africa. However, this finding was not consistent on the additive scale, when accounting for multiple comparisons or when using other definitions of malaria and malnutrition.
The investigators concluded pregnant women with malnutrition and malaria infection are at increased risk of low birthweight compared to women with only 1 risk factor or none, but malaria and malnutrition do not act synergistically.
Original title:
Malaria, malnutrition, and birthweight: A meta-analysis using individual participant data by Cates JE, Unger HW, […], Rogerson S.
Link:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5549702/
Additional information of El Mondo:
Find more information/studies on food fortification/malnutrition and pregnancy right here.