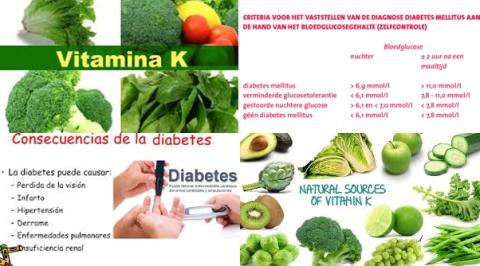
88 µg/d vitamin D supplementation reduces type 2 diabetes
Objectives:
Diabetes prevention is a public health priority. Vitamin D supplementation may help prevent the development of diabetes in persons at increased risk. Therefore, this review article has been conducted.
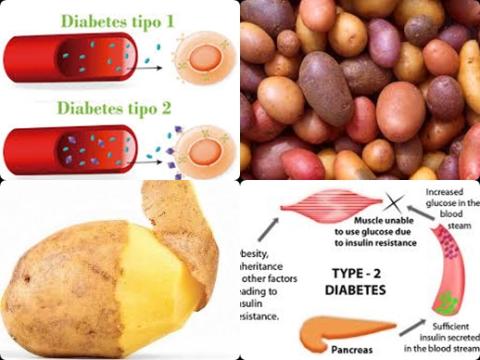
Does vitamin D supplementation reduce risk of type 2 diabetes?
Study design:
This review article included 28 RCTs with 3,848 participants.
The sample size varied from 23 to 511.
The mean age of participants ranged from 26 years to 71 years.
The duration of follow-up across studies ranged from 2 months to 5 years, with a median follow-up of 22 weeks [interquartile range (IQR): 14 to 48 weeks], a duration long enough to detect changes in measured outcomes.
The average vitamin D supplementation dose of 88 µg/d (3500 IU/d).
All included trials measured the effect of vitamin D supplementation on serum 25(OH)D concentrations.
Results and conclusions:
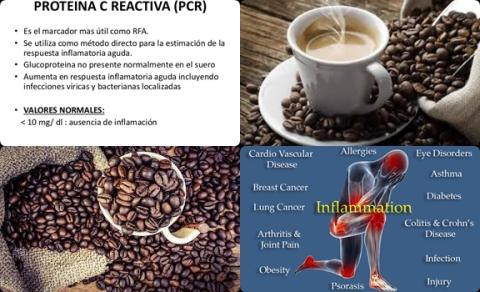
The investigators found overall, serum 25(OH)D concentrations in the treated arms (vitamin D-supplemented groups) significantly improved by 45.1 nmol/L [95% CI = 41.3 to 48.9, p 0.001, I2 = 97.4%].
The investigators found compared with the control group, vitamin D supplementation significantly reduced HbA1c level by -0.48% [95% CI = -0.79 to -0.18, p = 0.002, I2 = 92.1%].
However, after adjusting the effect size for potential publication bias using the “trim and fill” method, 4 potentially missing studies were imputed in the funnel plot and the effect size increased from -0.48% [95% CI = -0.79 to -0.18] to -0.71% [95% CI = -1.02 to -0.39].
The investigators found compared with the control group, vitamin D supplementation significantly reduced fasting plasma glucose level by -0.46 mmol/L [95% CI = -0.74 to -0.19, p = 0.001, I2 = 92.4%].
However, after adjusting the effect size for potential publication bias using the “trim and fill” method, 6 potentially missing studies were imputed in the funnel plot and the effect size increased -0.46 mmol/L [95% CI = -0.74 to 0.19] to -0.72 mmol/L [95% CI =-1.02 to -0.42].
The investigators found compared with the control group, vitamin D supplementation significantly reduced HOMA-IR level by -0.39 [95% CI = -0.68 to -0.11, p = 0.007, I2 = 91.3%].
However, after adjusting the effect size for potential publication bias using the “trim and fill” method, 5 potentially missing studies were imputed in the funnel plot and the effect size increased from -0.39 [95% CI = -0.68 to -0.11] to -0.62 [95% CI = -0.92 to -0.32].
The investigators found in subgroup analysis both HbA1c and HOMA-IR showed a greater reduction over time among overweight/obese individuals compared with prediabetics [HbA1c = -0.98 ± 0.45 vs -0.29 ± 0.14, p = 0.1 and HOMA-IR = -0.62 ± 0.23 vs -0.07 ± 0.16, p = 0.05].
The investigators found in subgroup analysis vitamin D supplementation significantly decreased HbA1c [p = 0.05], fasting plasma glucose level [p = 0.05] and HOMA-IR [p = 0.1] to a greater extent when serum 25(OH)D concentration achieved was above 86 nmol/L.
The investigators found in subgroup analysis vitamin D supplementation for less than 6 months provided a larger effect size on HbA1c in comparison with long durations [-0.75 ± 0.33 vs -0.25 ± 0.11, p = 0.1].
The investigators found in subgroup analysis HbA1c showed greater improvement in populations with a mean age younger than 45 years in comparison with older populations [-1.15 ± 0.6 vs -0.30 ± 0.1, p = 0.05].
The investigators found in subgroup analysis greater reductions were found within HbA1c and fasting plasma glucose levels when baseline (at the beginning of the study) mean serum 25(OH)D concentration was ≥50 nmol/L, whereas the lowering effect was significantly less in the subgroup with baseline mean 25(OH)D 50 nmol/L [HbA1c = -0.79 ± 0.25 vs -0.14 ± 0.13, p = 0.04 and fasting plasma glucose level = -0.69 ± 0.21 vs -0.11 ± 0.10, p = 0.05].
The investigators concluded 88 µg/d vitamin D supplementation during 22 weeks improves glycemic measures and insulin sensitivity and may be useful as part of a preventive strategy for type 2 diabetes, particularly among overweight/obese individuals younger than 45 years.
Original title:
Vitamin D Supplementation, Glycemic Control, and Insulin Resistance in Prediabetics: A Meta-Analysis by Mirhosseini N, Vatanparast H, [...], Kimball SM.
Link:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6016617/
Additional information of El Mondo:
Find more information/studies on diabetes and vitamin D right here.
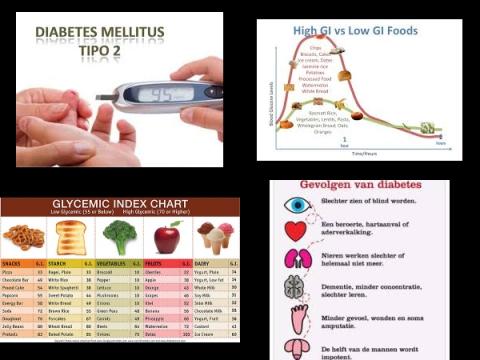
HbA1c, FPG, HOMA-IR and plasma glucose after 2-hour oral glucose tolerance test (2HPG) are different parameters associated with (pre)diabetes.