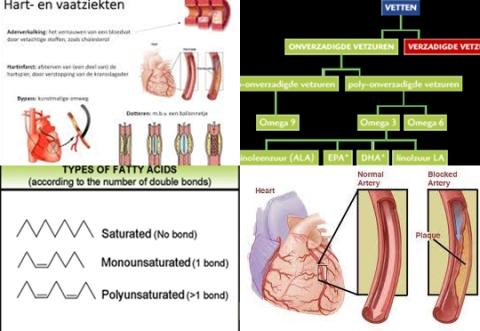
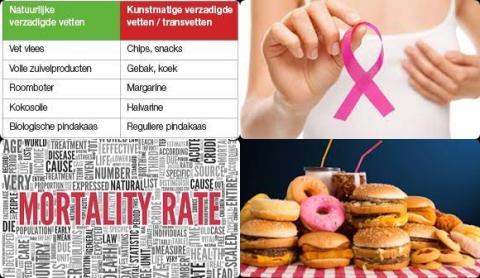
Saturated fat increases breast cancer mortality among women
Objectives:
The influence of dietary fat upon breast cancer mortality remains largely understudied despite extensive investigation into its influence upon breast cancer risk. Therefore, this review article has been conducted.
Does higher total fat or saturated fat dietary intake increase risk of breast-cancer-specific death (breast cancer mortality) among women?
Study design:
This review article included 15 prospective cohort studies investigating total fat and/or saturated fat intake (g/day) and breast cancer mortality.
Results and conclusions:
The investigators found there was no difference in risk of breast-cancer-specific death [HR = 1.14, 95% CI = 0.86 to 1.52, p = 0.34, n = 6] or all-cause death [HR = 1.73, 95% CI = 0.82 to 3.66, p = 0.15, n = 4] for women in the highest versus lowest category of total fat dietary intake.
No difference because HR of 1 was found in the 95% CI of 0.82 to 3.66. HR of 1 means no risk/association.
The investigators found for the highest versus lowest category of saturated fat dietary intake, a significantly increased risk of 51% for breast-cancer-specific death among women [HR = 1.51, 95% CI = 1.09 to 2.09, p 0.01 n = 4].
Significant because HR of 1 was not found in the 95% CI of 1.09 to 2.09. HR of 1 means no risk/association.
The investigators concluded that higher saturated fat dietary intake increases risk of breast-cancer-specific death among women.
Original title:
Dietary fat and breast cancer mortality: A systematic review and meta-analysis by Brennan SF, Woodside JV, […], Cantwell MM.
Link:
https://pubmed.ncbi.nlm.nih.gov/25692500/
Additional information of El Mondo:
Find more information/studies on fat consumption and breast cancer right here.
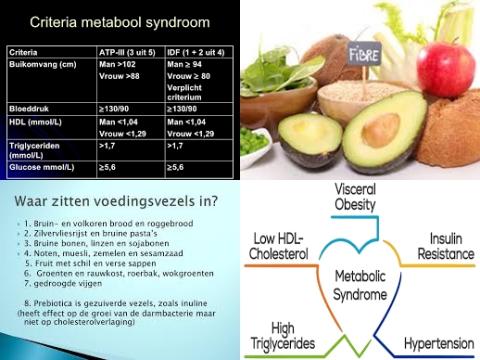
A diet high in saturated fat is a diet with more than 10 En% saturated fat.
The most easy way to follow a diet with more than 10 En% saturated fat is to choose only meals/products with more than 10 En% saturated fat. Check here which products contain more than 10 En% saturated fat.
However, the most practical way to follow a diet with more than 10 En% saturated fat is, all meals/products that you eat on a daily basis should contain on average more than 10 En% saturated fat.
To do this, use the 7-points nutritional profile app to see whether your daily diet contains more than 10 En% saturated fat.
However, a diet with more than 10 En% saturated fat is an unhealthy diet.
A diet low in saturated fat is a diet with maximum 7 En% saturated fat.