Objectives:
Several B vitamins are essential in the one-carbon metabolism pathway, which is central to DNA methylation, synthesis and repair. Moreover, an imbalance in this pathway has been linked to certain types of cancers. Therefore, this review article has been conducted.
Is there a relationship between dietary vitamin intake and risk of esophageal cancer (EC)?
Study design:
This review article included 24 patient-control studies and 2 cohort studies with a total of 510,954 participants and 6,404 esophageal cancer cases, which included 1,919 esophageal adenocarcinoma (EAC) patients, 2,010 esophageal squamous cell carcinoma (ESCC) patients and 2,475 esophageal cancer (EC) patients.
The quality scores of all studies ranged from 6 to 8, with a median score of 7.
There was no significant publication bias in the final analysis with respect to vitamin B2 [p = 0.244], vitamin B6 [p = 0.068], folate [p = 0.054] or vitamin B12 [p = 0.093].
A sensitivity analysis revealed that no individual study affected the pooled effect size.
Results and conclusions:
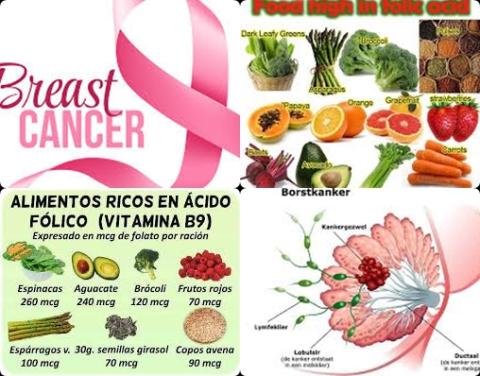
The investigators found for the highest level versus the lowest level of dietary folate intake, a significantly reduced risk of 38% [pooled OR = 0.62, 95% CI = 0.56-0.68, I2 = 40.2%] for esophageal cancer.
Subgroup analysis revealed that this inverse correlation (reduced risk) was present in the US [OR = 0.58, 95% CI = 0.51-0.67], Europe [OR = 0.51, 95% CI = 0.40-0.65] and Australia [OR = 0.74, 95% CI = 0.58-0.95], but not in Asia [OR = 0.77, 95% CI = 0.59-1.01].
The investigators found in dose-response analysis that each 100 μg/day increase in dietary folate intake significantly reduced the risk of esophageal cancer by 12% [OR = 0.88, 95% CI = 0.86-0.91].
Significant means that there is an association with a 95% confidence.
The investigators found for the highest level versus the lowest level of dietary vitamin B6 intake, a significantly reduced risk of 41% [pooled OR = 0.59, 95% CI = 0.52-0.66, I2 = 46.8%] for esophageal cancer.
This inverse relationship remained significant in subgroup analyses for esophageal adenocarcinoma [OR = 0.58, 95% CI = 0.49-0.68] and esophageal squamous cell carcinoma [OR = 0.47, 95% CI = 0.33-0.67].
The investigators found in dose-response analysis, a significantly reduced risk of 18% [OR = 0.82, 95% CI = 0.76-0.88] for esophageal cancer for 2.0 mg/day of dietary vitamin B6 intake.
The investigators found in dose-response analysis, a significantly reduced risk of 33% [OR = 0.67, 95% CI = 0.59-0.75] for esophageal cancer for 2.5 mg/day of dietary vitamin B6 intake.
The investigators found in dose-response analysis, a significantly reduced risk of 45% [OR = 0.55, 95% CI = 0.44-0.67] for esophageal cancer for 3.0 mg/day of dietary vitamin B6 intake.
The investigators found in dose-response analysis that each 1 mg/day increase in dietary B6 increase significantly reduced the risk of esophageal cancer by 16% [OR = 0.84, 95% CI = 0.80-0.89].
The investigators found for the highest level versus the lowest level of dietary vitamin B12 intake, a significantly increased risk of 30% [pooled OR = 1.30, 95% CI = 1.05-1.62, I2 = 73.5%] for esophageal cancer.
A subgroup analysis based on geographic location revealed similar results in the US [OR = 1.26, 95% CI = 1.03-1.53] and Europe [OR = 2.54, 95% CI = 1.16-5.53], but not in Australia [OR = 0.93, 95% CI = 0.73-1.19].
A subgroup analysis based on histological type revealed that this correlation was present among patients with esophageal adenocarcinoma [OR = 1.47, 95% CI = 1.02-2.11], but not among patients with esophageal squamous cell carcinoma [OR = 1.00, 95% CI = 0.63-1.61].
The investigators found in dose-response analysis that each 1 μg/day increase in dietary B12 intake significantly increased the risk of esophageal cancer by 2% [OR = 1.02, 95% CI = 1.00-1.03].
The investigators concluded that both dietary vitamin B6 intake (at least 1 mg/day) and dietary folate intake (at least 100 μg/day) are inversely correlated with esophageal cancer risk, whereas dietary vitamin B12 intake (at least 1 μg/day) increases esophageal cancer risk.
Original title:
Intake of Dietary One-Carbon Metabolism-Related B Vitamins and the Risk of Esophageal Cancer: A Dose-Response Meta-Analysis by Qiang Y, Li Q, […], Wang F.
Link:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6073467/
Additional information of El Mondo:
Find more information/studies on folate, vitamin B6 and B12 and cancer right here.