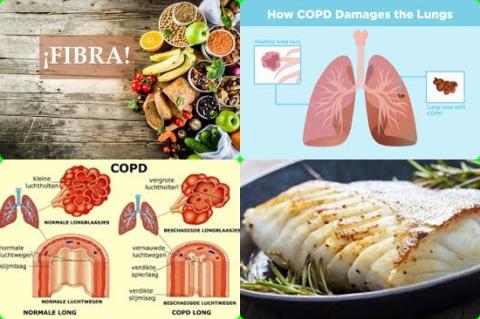
Serum albumin concentrations are lower in patients with stable COPD
Objectives:
Are serum albumin concentrations lower in patients with stable COPD compared to non-COPD controls?
Study design:
This review article included 26 studies with a total of 2,554 COPD patients (74% males) and 2,055 non-COPD controls (63% males).
Overall, the mean age of participants across all studies was 61.7 years in COPD patients and 64.6 years in controls (patients without COPD).
Almost all (24 out of 26) were prospective cohort studies.
The Begg’s [p = 0.04] and Egger’s tests [p = 0.01] showed a significant publication bias; however, the trim-and-fill analysis found that no study was missing or should be added.
Results and conclusions:
The investigators found pooled results showed that serum albumin concentrations were significantly lower in COPD patients [SMD = -0.50, 95% CI = -0.67 to -0.32, p 0.001, I2 = 85.7%, p 0.001] .
Sensitivity analysis showed that the effect size was not modified when any single study was in turn removed [effect size ranged between -0.44 and -0.52].
The investigators found no significant differences in SMD of serum albumin concentrations between COPD patients with forced expiratory volume in the 1st second (FEV1) 50% and those with FEV1 > 50%.
The investigators concluded that serum albumin concentrations are lower in patients with stable COPD compared to non-COPD controls. This supports the presence of a deficit in systemic anti-inflammatory and antioxidant defense mechanisms in COPD.
Original title:
Serum Albumin Concentrations in Stable Chronic Obstructive Pulmonary Disease: A Systematic Review and Meta-Analysis by Zinellu E, Fois AG, […], Pirina P.
Link:
https://www.mdpi.com/2077-0383/10/2/269/htm
Additional information of El Mondo:
Find here more information/studies about review article/significant and chronic diseases.