Objectives:
Despite growing evidence for food-based dietary patterns' potential to reduce cardiovascular disease risk, knowledge about the amounts of food associated with the greatest change in risk of specific cardiovascular outcomes and about the quality of meta-evidence is limited. Therefore, this review article (meta-analysis) has been conducted.
Which food-based dietary patterns reduce risk of cardiovascular diseases, such as coronary heart disease (CHD), stroke and heart failure (HF)?
Study design:
This review article included 123 prospective cohort studies.
Results and conclusions:
The investigators found whole grains significantly reduced risk of coronary heart disease with 5% [RR = 0.95, 95% CI = 0.92-0.98]. Significantly means that there is an association with a 95% confidence.
The investigators found whole grains significantly reduced risk of heart failure with 4% [RR = 0.96, 95% CI = 0.95-0.97]. Significantly because RR of 1 was not found in the 95% CI of 0.95 to 0.97. RR of 1 means no risk/association.
The investigators found vegetables significantly reduced risk of coronary heart disease with 3% [RR = 0.97, 95% CI = 0.96-0.99]. Significantly means it can be said with a 95% confidence that a intake of vegetables really decreased the risk of getting coronary heart disease with 3%.
The investigators found fruits significantly reduced risk of coronary heart disease with 6% [RR = 0.94, 95% CI = 0.90-0.97].
The investigators found vegetables significantly reduced risk of stroke with 8% [RR = 0.92, 95% CI = 0.86-0.98].
The investigators found fruits significantly reduced risk of stroke with 10% [RR = 0.90, 95% CI = 0.84-0.97].
The investigators found nuts non-significantly reduced risk of coronary heart disease with 33% [RR = 0.67, 95% CI = 0.43-1.05]. Non-significantly means that there is no association with a 95% confidence.
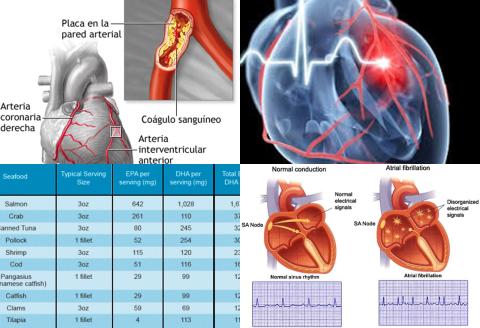
The investigators found fish consumption significantly reduced risk of stroke with 14% [RR = 0.86, 95% CI = 0.75-0.99].
The investigators found fish consumption significantly reduced risk of heart failure with 20% [RR = 0.80, 95% CI = 0.67-0.95].
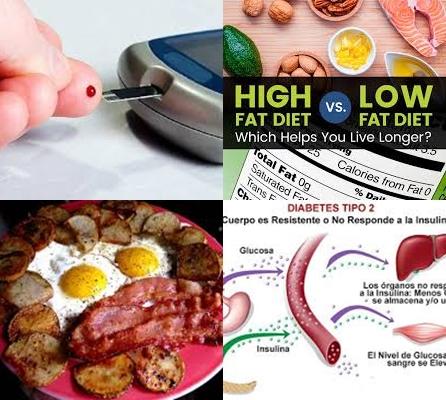
The investigators found egg significantly increased risk of heart failure with 16% [RR = 1.16, 95% CI = 1.03-1.31].
The investigators found red meat significantly increased risk of coronary heart disease with 15% [RR = 1.15, 95% CI = 1.08-1.23].
The investigators found red meat significantly increased risk of stroke with 12% [RR = 1.12, 95% CI = 1.06-1.17].
The investigators found red meat significantly increased risk of heart failure with 8% [RR = 1.08, 95% CI = 1.02-1.14].
The investigators found processed meat significantly increased risk of coronary heart disease with 27% [RR = 1.27, 95% CI = 1.09-1.49].
The investigators found processed meat significantly increased risk of stroke with 17% [RR = 1.17, 95% CI = 1.02-1.34].
The investigators found processed meat significantly increased risk of heart failure with 12% [RR = 1.12, 95% CI = 1.05-1.19].
The investigators found sugar-sweetened beverages significantly increased risk of coronary heart disease with 17% [RR = 1.17, 95% CI = 1.11-1.23].
The investigators found sugar-sweetened beverages significantly increased risk of heart failure with 7% [RR = 1.07, 95% CI = 1.02-1.12].
The investigators found sugar-sweetened beverages significantly increased risk of stroke with 8% [RR = 1.08, 95% CI = 1.05-1.12].
The investigators found there were clear indications for non-linear dose-response relationships between whole grains, fruit, nuts, dairy and red meat and coronary heart disease.
The investigators concluded there is a relationship between food-based dietary patterns and risk of cardiovascular diseases, with an increased risk for consumption of eggs, red meat, processed meat and sugar-sweetened beverages and a decreased risk for consumption of whole grains, vegetables, fruit and fish.
Original title:
Food groups and risk of coronary heart disease, stroke and heart failure: A systematic review and dose-response meta-analysis of prospective studies by Bechthold A, Boeing H, […], Schwingshackl L.
Link:
https://www.ncbi.nlm.nih.gov/pubmed/29039970
Additional information of El Mondo:
Find more information/studies on food groups and cardiovascular diseases right here.