Objectives:
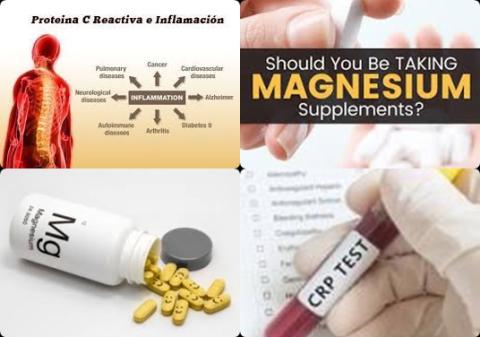
Does magnesium supplementation reduce C-reactive protein concentrations in humans?
Study design:
This review article included 8 RCTs (2004-2014) with 349 participants.
The mean age of participants ranged from 18 to 85 years.
The range of duration of the supplementation intervention across studies was from 8 h to 6.5 months.
The consumed range of magnesium dose in these studies was from 320 to 1500 mg/day. The baseline level (at the start of the study) of the CRP varied between the studies from 0.42 mg/dL as minimum to 9.4 mg/dL as maximum.
Results and conclusions:
The investigators found magnesium supplementation significantly reduced serum CRP levels [WMD = -1.33 mg/dL, 95% CI = -2.63 to -0.02, p 0.001, I2 = 29.1%, p 0.123] across all studies.
In leave-one-out sensitivity analyses, the pooled effect estimates remained similar across all studies for CRP levels [WMD = -1.33 mg/dL, 95% CI = -2.63 to -0.02].
The investigators found after adjustment of the effect size for potential publication bias using the “trim and fill” correction, no potentially missing studies were imputed in the funnel plot [WMD = -1.33 mg/dL, 95% CI = -2.63 to -0.02]. The “fail-safe N” test showed that 146 studies would be needed to bring the WMD down to a non-significant [p > 0.05] value.
The investigators found in random-effects meta-regression changes in serum CRP levels were independent of the dosage of magnesium [slope = -0.004, 95% CI = -0.03 to 0.02, p = 0.720, and duration [slope = -0.06, 95% CI = -0.37 to 0.24, p = 0.681] of supplementation.
The investigators found in 4 RCTs that subjects with a baseline CRP of ≥ 2 mg/dL had more significant reduction in the serum CRP level [WMD = -2.95 mg/dL, 95% CI = -3.35 to -2.25, p 0.001, I2 = 1.1%, p = 0.952] compared with subjects with a baseline CRP of 2 mg/dL [WMD = -0.23 mg/dL, 95% CI = -0.195 to -0.326, p 0.001, I2 = 1.3% p = 0.923].
The investigators found magnesium supplementation non-significantly reduced IL-6 levels [WMD = -0.16 pg/dL, 95% CI = -3.52 to 3.26, p = 0.236, I2 = 2.3%, p = 0.802] across all studies.
The investigators found magnesium supplementation significantly increased TNF-α levels [WMD = 1.97 pg/dL, 95% CI = 1.12 to 2.82, p = 0.043, I2 = 2.1%, p = 0.869] across all studies.
The investigators found magnesium supplementation non-significantly decreased fasting blood glucose (FBG) levels [WMD = -0.61 mg/dL, 95% CI = -2.72 to 1.48, p = 0.182, I2 = 6.1%, p = 0.742] across all studies.
The investigators found magnesium supplementation non-significantly decreased systolic blood pressure levels [WMD = -0.93 mmHg, 95% CI = -3.03 to 1.20, p = 0.293, I2 = 3.6%, p = 0.526] across all studies.
The investigators found magnesium supplementation non-significantly decreased diastolic blood pressure levels [WMD = -0.30 mmHg, 95% CI = -2.80 to 2.19, p = 0.639, I2 = 3.8%, p = 0.489] across all studies.
The investigators found magnesium supplementation non-significantly increased BMI levels [WMD = 0.27 kg/m2, 95% CI = -0.59 to 1.15, p = 0.542, I2 = 2.0%, p = 0.906] across all studies.
The investigators concluded that 320 to 1500 mg/day magnesium supplementation decreases serum CRP levels, especially with the baseline values ≥ 2 mg/dL. To provide more conclusive results and clarify the mechanistic pathways, RCTs with a larger sample size and a long-term follow-up period are warranted.
Original title:
Effect of magnesium supplements on serum C-reactive protein: a systematic review and meta-analysis by Mazidi M, Rezaie P and Banach M.
Link:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6040119/
Additional information of El Mondo:
Find more information/studies on magnesium and chronic diseases right here.