50g/day processed meat increase type 2 diabetes

Objectives:
Is there an association between total meat, red meat, processed meat, poultry and fish intake and risk of type 2 diabetes (T2D)?
Study design:
This review article included 28 prospective cohort studies.
Results and conclusions:
The investigators found when compared with the lowest category, the highest category of total meat intake, significantly increased risk of type 2 diabetes with 33% [summary relative risk = 1.33, 95% CI = 1.16 to 1.52].
Significantly means that there is an association with a 95% confidence.
The investigators found when compared with the lowest category, the highest category of red meat intake, significantly increased risk of type 2 diabetes with 22% [summary relative risk = 1.22, 95% CI = 1.16 to 1.28].
Significantly because summary relative risk of 1 was not found in the 95% CI of 1.16 to 1.28. Summary relative risk of 1 means no risk/association.
The investigators found when compared with the lowest category, the highest category of processed meat intake, significantly increased risk of type 2 diabetes with 25% [summary relative risk = 1.25, 95% CI = 1.13 to 1.37].
Significantly means it can be said with a 95% confidence that the highest category of processed meat intake really increased risk of type 2 diabetes with 25%.
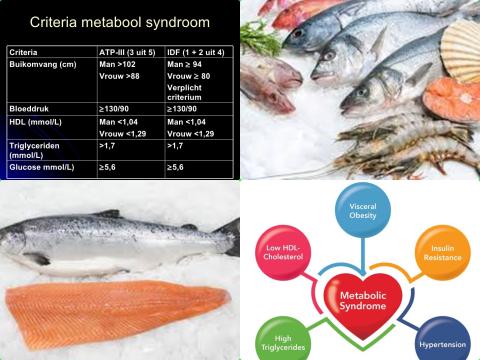
The investigators found no association between highest category of poultry intake and risk of type 2 diabetes [summary relative risk = 1.00, 95% CI = 0.93 to 1.07].
No association because summary relative risk of 1 was found in the 95% CI of 0.93 to 1.07. Summary relative risk of 1 means no risk/association.
The investigators found no association between highest category of fish intake and risk of type 2 diabetes [summary relative risk = 1.01, 95% CI = 0.93 to 1.10].
The investigators found in the dose-response analysis, each additional 100g/day of total and red meat and 50g/day of processed meat, were found to be associated with a 36% [95% CI = 1.23 to 1.49], 31% [95% CI = 1.19 to 1.45] and 46% [95% CI = 1.26 to 1.69] increased risk of type 2 diabetes, respectively.
The investigators found, in addition, there was evidence of a non-linear dose-response association between processed meat and type 2 diabetes [p = 0.004], with the risk increasing by 30% with increasing intakes up to 30g/day.
The investigators concluded 100g/day of total meat, 100g/day red meat and 50g/day of processed meat, increase risk of type 2 diabetes.
Original title:
Meat and fish intake and type 2 diabetes: dose-response meta-analysis of prospective cohort studies by Yang X, Li Y, […], Li L.
Link:
https://www.ncbi.nlm.nih.gov/pubmed/32302686
Additional information of El Mondo:
Find more information/studies on fish and meat consumption and diabetes right here.