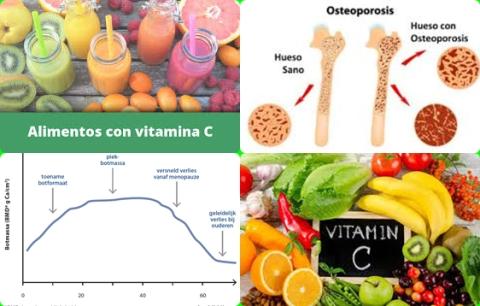
54 mg/day genistein increase bone mineral density in postmenopausal women
Objectives:
Isoflavones have a structure similar to 17β-estradiol, so they may be useful to postmenopausal women in preventing bone loss related to estrogen deficiency. Therefore, this review article has been conducted.
Do isoflavone supplements increase bone mineral density (BMD) in postmenopausal women?
Study design:
This review article included 63 RCTs, involving 6,427 postmenopausal women.
Isoflavone interventions were generally safe and well tolerated.
Results and conclusions:
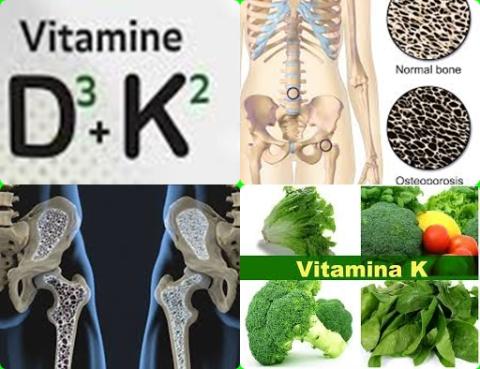
The investigators found statistically significant differences in bone mineral density at the last follow-up visit between the two groups (isoflavones vs. control) at the lumbar spine [MD = 21.34 mg/cm2, 95% CI = 8.21 to 34.47 mg/cm2, p = 0.001], the femoral neck [MD = 28.88 mg/cm2, 95% CI = 15.05 to 42.71 mg/cm2, p 0.0001] and the distal radius [MD = 19.27 mg/cm2, 95% CI = 5.65 to 32.89 mg/cm2, p = 0.006].
This improved bone mineral density was found for genistein 54 mg/day and ipriflavone (a synthetic isoflavone) 600 mg/day.
The investigators concluded isoflavone interventions, genistein (54 mg/day) and ipriflavone (600 mg/day) in particular, have beneficial effects on bone mineral density outcomes and are safe in postmenopausal women. They may be considered as a complementary or alternative option in the prevention and treatment of menopause-related osteoporosis.
Original title:
Effects of Isoflavone Interventions on Bone Mineral Density in Postmenopausal Women: A Systematic Review and Meta-Analysis of Randomized Controlled Trials by Sansai K, Takuathung MN, [...], Koonrungsesomboon N.
Link:
https://pubmed.ncbi.nlm.nih.gov/32524173/
Additional information of El Mondo:
Find more information/studies on isoflavones and elderly right here.