1.5 g/day garlic supplementation reduces adiponectin level among participants ˂30 years

Objectives:
Does garlic supplementation reduce adiponectin and leptin serum levels?
Study design:
This review article included 5 RCTs.
Results and conclusions:
The investigators found that garlic supplementation did not significantly affect adiponectin [Hedges's = 0.20, 95% CI = -0.06 to 0.47, p = 0.12] and leptin [Hedges's = 0.08, 95% CI = -0.26 to 0.41, p = 0.65] concentrations in comparison with placebo.
The investigators found, however, in the subgroup analysis, significantly increased serum adiponectin level was seen following garlic supplementation in trials with a mean age of participants ˂30 years [Hedges's = 0.44, 95% CI = 0.01 to 0.87, p = 0.04], the doses ˂1.5 g/day [Hedges's = 0.38, 95% CI = 0.02 to 0.71, p = 0.04] and trials with duration ≥8 weeks [Hedges's = 0.48, 95% CI = 0.08 to 0.89, p = 0.02].
The investigators concluded that ˂1.5 g/day garlic supplementation during ≥8 weeks reduces adiponectin level among participants ˂30 years.
Original title:
Systematic review and meta-analysis of randomized, controlled trials on the effects of garlic supplementation on serum adiponectin and leptin levels by Shekarchizadeh-Esfahani P, Hassani B, […], Soraya N.
Link:
https://pubmed.ncbi.nlm.nih.gov/33792129/
Additional information of El Mondo:
Find here more information/studies about review article/significant and garlic.
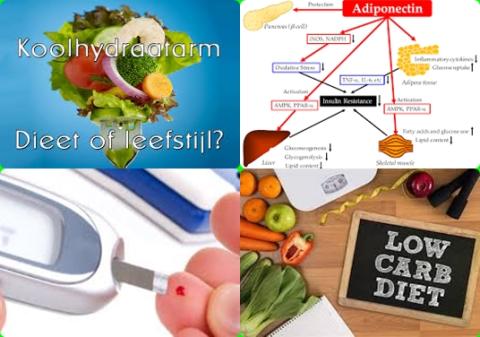
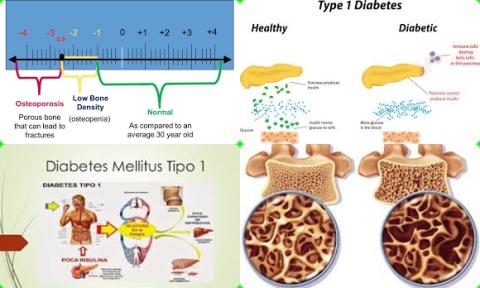
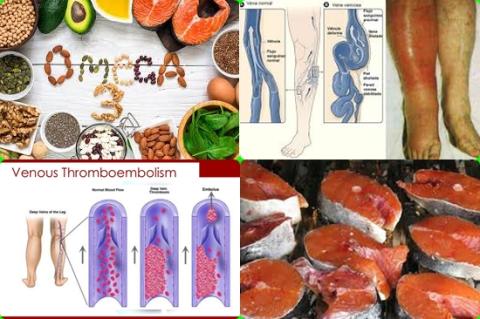
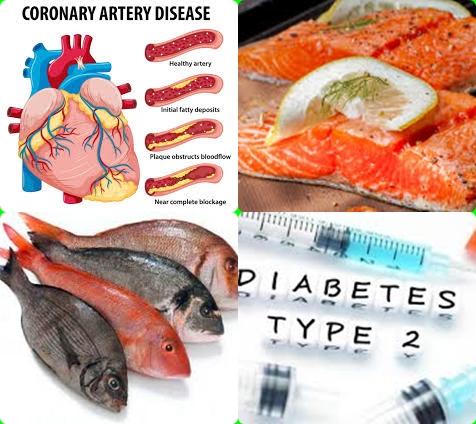
Adiponectin is a fat-derived hormone that appears to play a crucial role in protecting against insulin resistance/diabetes and atherosclerosis (atherosclerosis is the dominant cause of cardiovascular disease (CVD)). Decreased adiponectin levels are thought to play a central role in the development of obesity, cardiovascular disease and type 2 diabetes in humans.