Objectives:
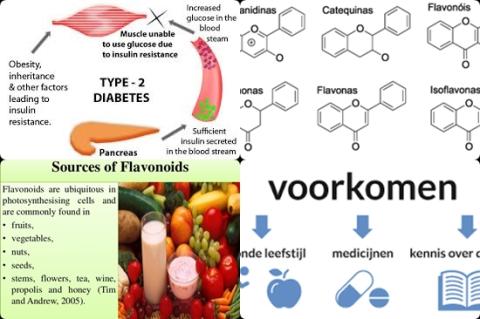
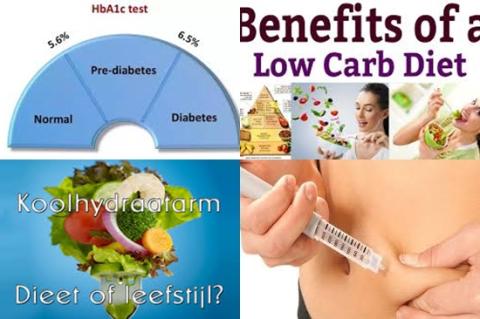
Epidemiological studies exploring the role of flavonoids intake in preventing type 2 diabetes mellitus (T2DM) showed inconsistent results. Therefore, this review article (meta-analysis) has been conducted.
Does flavonoids intake decrease risk of developing type 2 diabetes?
Study design:
This review article included 10 independent cohorts published between 2002 and 2017 with a total of 312,015 participants, of which 19,953 type 2 diabetes cases were identified during the follow-up periods from 4 to 28 years.
All participants were free of type 2 diabetes at baseline (at the beginning of the study), with age ranging from 28 to 75 years.
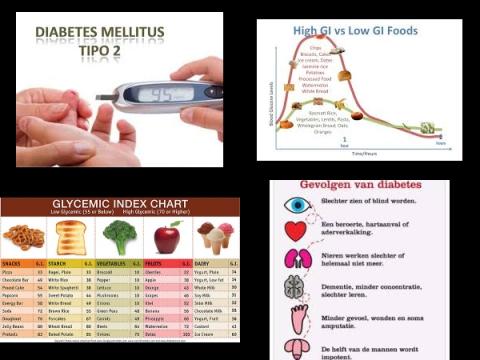
Dietary flavonoids intake was evaluated using food-frequency questionnaire and type 2 diabetes was frequently ascertained through medical records.
In the original studies, the median intake level of total flavonoids was 8.9 to 501.8 mg/day for the lowest categories and 33.2 to 1452.3 mg/day for the highest categories.
The most commonly adjusted variables included age, sex, total energy intake, body mass index, smoking, alcohol consumption and physical activity.
All included studies had a NOS score of ≥7, with an average score of 7.9, indicating the presence of high methodological quality.
There was no indication of publication bias from visual inspection of the funnel plot, which was further confirmed by Egger test [p = 0.253].
Results and conclusions:
The investigators found when compared with the lowest intake, the highest intake of total flavonoids was associated with a significantly 9% decreased risk of type 2 diabetes [RR = 0.91, 95% CI = 0.86-0.96, I2 = 21%, p = 0.257].
In stratified analyses, the pooled RR for total flavonoids intake was not modified by sample size, sex, follow-up duration and study location.
Leave-one-out sensitivity analysis showed that no individual study had a significant influence on the final result.
The investigators found in subgroup analyses when compared with the lowest intake, the highest intake of anthocyanidins significantly decreased risk of type 2 diabetes with 11% [RR = 0.89, 95% CI = 0.82-0.95].
The investigators found in subgroup analyses when compared with the lowest intake, the highest intake of flavan-3-ols significantly decreased risk of type 2 diabetes with 14% [RR = 0.86, 95% CI = 0.78-0.95].
The investigators found in subgroup analyses when compared with the lowest intake, the highest intake of flavonols significantly decreased risk of type 2 diabetes with 14% [RR = 0.86, 95% CI = 0.80-0.94].
The investigators found in subgroup analyses when compared with the lowest intake, the highest intake of isoflavones significantly decreased risk of type 2 diabetes with 9% [RR = 0.91, 95% CI = 0.84-0.98].
The investigators found in 9 cohort studies a curvilinear relationship between total flavonoids intake and type 2 diabetes risk [p for nonlinearity = 0.042] with a significant risk reduction at an intake of ≥550 mg/day.
The investigators found when assuming a linear association, the risk of type 2 diabetes was reduced by 5% [RR = 0.95, 95% CI = 0.93-0.97] for each 300-mg/day increment in total flavonoids intake.
The investigators concluded that intakes of total flavonoids, particularly ≥550 mg/day, anthocyanidins, flavan-3-ols, flavonols and isoflavones are associated with significantly decreased risks of type 2 diabetes in the highest versus lowest analyses. Additionally, the dose-response analysis suggest a curvilinear relationship of total flavonoids intake with type 2 diabetes risk; when assuming a linear manner, the risk of type 2 diabetes is reduced by 5% for an increment of 300 mg/day in total flavonoids intake.
Original title:
Flavonoids intake and risk of type 2 diabetes mellitus: A meta-analysis of prospective cohort studies by Xu H, Luo J, [...], Wen Q.
Link:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5959406/
Additional information of El Mondo:
Find more information/studies on diabetes and flavonoids right here.
|
Flavonols
|
Flavan-3-ols
|
Flavones
|
Flavonones
|
Anthocyanidins
|
|
onions
|
apples
|
parsley
|
oranges
|
blueberries
|
|
apples
|
bananas
|
bell peppers
|
grapefruit
|
bananas
|
|
romaine lettuce
|
blueberries
|
celery
|
lemons
|
strawberries
|
|
tomatoes
|
peaches
|
apples
|
tomatoes
|
cherries
|
|
garbanzo beans
|
pears
|
oranges
|
|
pears
|
|
almonds
|
strawberries
|
watermelon
|
|
cabbage
|
|
turnip greens
|
|
chili peppers
|
|
cranberries
|
|
sweet potatoes
|
|
cantaloupe
|
|
plums
|
|
quinoa
|
|
lettuce
|
|
raspberries
|
|
|
|
|
|
garbanzo beans
|
|
Food items
|
Flavonoid content (mg)
|
|
Blueberry (100g)
|
25-500
|
|
Black currant (100g)
|
130-400
|
|
Strawberry (200g)
|
30-150
|